‘On fire’ with sJIA: When arthritis is much more than joint pain

Georgia is finally living her best life. Her toddler years were challenging: At 15 months old, a series of high fevers landed her at Boston Children’s Hospital for two weeks. After many rounds of tests looking for infection and a bone marrow biopsy to rule out cancer, she was diagnosed with systemic juvenile idiopathic arthritis (sJIA), a rare childhood arthritis.
There’s a misconception that arthritis is just something that happens to older people’s joints. While Georgia did often have sore joints, her primary symptoms were “high-spiking fevers and general misery,” says Georgia’s mother Sabrina. “She didn’t want to eat, she didn’t want to move. But the important piece was what we couldn’t see — her lab results for inflammatory markers were off the charts.”
Inflammation throughout the body is the hallmark of sJIA. Even worse, Georgia’s form of the disease has been complicated by macrophage activation syndrome (MAS). In MAS, inflammation runs rampant in the body, not unlike what happens sometimes with COVID-19 and multisystem inflammatory syndrome in children (MIS-C). MAS is life-threatening and has landed Georgia at Boston Children’s, including the intensive care unit, many times.
“She was on fire,” says Sabrina.
Calming the immune system in sJIA
Systemic JIA (also called Still’s disease) has historically been the hardest form of childhood arthritis to treat. The key is to tamp down inflammation, which can eventually damage multiple organs like the heart, lungs, and liver as well as the joints.
For two years, we could not get things to calm down. But the doctors always had another option to try. I really clung to that.”
For years, Georgia endured high doses of steroids, which curbed the inflammation but also curtailed her growth. She also received daily injections of biologic drugs, protein drugs that block the different signals that trigger inflammation, such as IL-1. Georgia’s doctors, Mary Beth Son, MD and Pui Lee, MD, PhD in the Rheumatology Program, have changed the biologics several times when they stopped working or, in one instance, caused an allergic reaction.
That trial-and-error approach is typical in rheumatology, where every case is different and the best treatment is often a guess. “For two years, we could not get things to calm down,” says Sabrina. “But the doctors always had another option to try. I really clung to that. We tethered ourselves to them, they were the captains of our ship, our north star.”
A new set of challenges
Now 10 and in the fourth grade, Georgia is stable on methotrexate, an immune-suppressing drug, plus a relatively new biologic drug, canakinumab, that requires a shot only every six weeks. About 18 months ago, she was able to discontinue taking steroids.
Because her immune system is suppressed, Georgia and her family have to avoid exposure to infections. At school, Georgia sits out during gym to avoid germs and brings her own water from home. But she’s feeling well, taking horseback lessons, playing soccer, and skiing with her family.
“Right now we’re in a place where her day-to-day is pretty normal,” says Rob, Georgia’s father. “But now that she’s stable, in some ways it’s more complicated.”
Though she shows no outward signs, the constant low-level inflammation caused by sJIA remains a threat to Georgia’s internal organs. She has been found to have interstitial lung disease, so far mild, and is being followed for potential heart and eye complications.
“There’s a question of how things will go later on,” Dr. Lee says. “Georgia’s lung disease is progressing slowly now, but at some point we may have to use a different medicine.”
A new sJIA treatment?
No new drug classes have been developed for sJIA since Boston Children’s rheumatologists helped establish biologics as a first line of treatment about a decade ago. Despite this advance, 20 to 30 percent of children receiving biologics have ongoing inflammation and sometimes develop MAS.
We use MTORC1 inhibitors pretty comfortably, so it wouldn’t be far-fetched for us to try them for sJIA under careful observation.”
But based on their lab research, Dr. Lee and Peter Nigrovic, MD, Boston Children’s chief of Immunology, may now have another option in their back pocket should Georgia’s inflammation increase.
Studying mice that produce excess amounts of the inflammatory signal IL-1, leading to features of sJIA, Dr. Lee noticed that a complex of proteins called MTORC1 seemed be at the hub of inflammation. His lab created a new mouse model with excess MTORC1 signaling and found that the mice developed features of both sJIA and MAS.
“When MTORC1 signaling was especially strong, the mice would develop MAS in addition to features of sJIA,” notes Dr. Lee.
Cells from people with sJIA, especially those with MAS, also showed prominent MTORC1 activity. And when Dr. Lee and Dr. Nigrovic’s team blocked MTORC1 in the mice, they saw reduced inflammation and reduced arthritis severity.
Could blocking MTORC1 help people with severe sJIA? Drs. Lee and Nigrovic hope it will. MTORC1 inhibitors like rapamycin and sirolimus have been found safe and are already used for various diseases involving immune dysfunction as well as some cancers. And unlike biologics, they can be given orally, with no need for injections.
“We use these drugs pretty comfortably, so it wouldn’t be far-fetched for us to try them under careful observation when nothing else is working out, or when the more expensive biologic drugs are unavailable,” says Dr. Nigrovic. “If that’s successful, we would need to treat more patients and report the results to build an evidence base. That could possibly spur clinical trials.”
‘Everyone has fear, but I won’t let it control me’
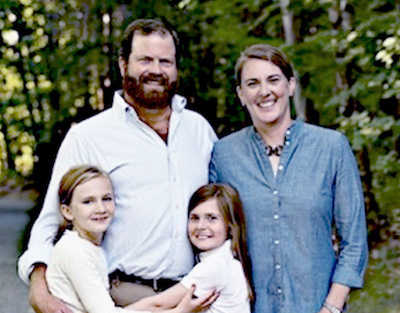
Georgia isn’t letting her condition dictate her life, though her parents and doctors are keeping watch. An advocate for the Arthritis Foundation, Georgia will soon take part in a 5K “Jingle Bell” fundraiser for research. Her motto is, “Everyone has fear, but I won’t let it control me.”
“We are so fortunate to live near a pediatric hospital where doctors have seen cases like Georgia’s,” says Sabrina, who has served on Boston Children’s Family Advisory Council. “And we’re so grateful that there are smart, dedicated people like Dr. Lee studying this disease.”
Learn more about the Rheumatology Program and why we lead in research.
Related Posts :
-

A global view of rheumatic disease during COVID-19
COVID-19 is bringing new challenges to many people with underlying rheumatic disease who already are immunocompromised by the very nature ...
-

How COVID-19 triggers massive inflammation
Why do some people with COVID-19 develop severe inflammation, leading to respiratory distress and damage to multiple organs? A new ...
-

Trusting their instincts: Gary’s parents find help for immune-mediated hepatitis
For Mercedes Hollingsworth and Gary Walker, Jr., trusting their parental instincts helped get their son Gary Walker III — affectionately known ...
-

Targeting a rogue T cell prevents and reverses multiple sclerosis in mice
Multiple sclerosis is an autoimmune disease affecting both adults and children. It’s driven by “helper” T cells, white blood ...