Trusting their instincts: Gary’s parents find help for immune-mediated hepatitis
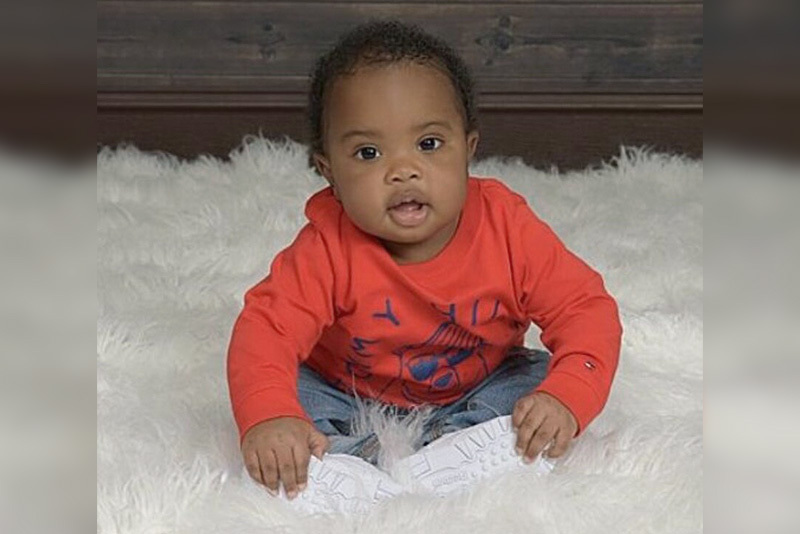
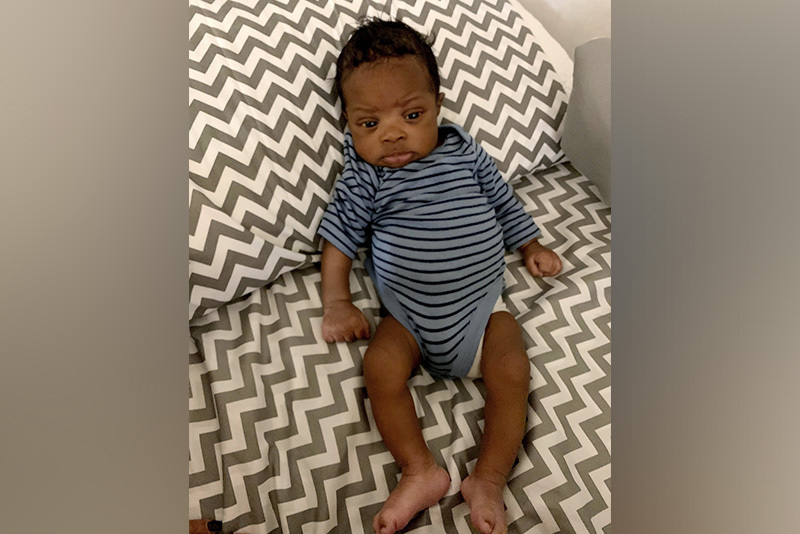
For Mercedes Hollingsworth and Gary Walker, Jr., trusting their parental instincts helped get their son Gary Walker III — affectionately known as GW — the care he needed. “We knew right away that something wasn’t right,” she says. “He just wasn’t a happy newborn. He looked miserable all the time.”
Mercedes, who also has an older son, wasn’t a new parent. But when she and Gary brought their concerns to GW’s pediatrician, they didn’t feel heard. Although GW’s skin and eyes had developed a yellow tinge, the doctor told them not to worry.
“They thought it was breastfeeding jaundice and said he was fine,” she remembers. Breastfeeding jaundice typically occurs when a baby doesn’t take in enough breast milk to meet their nutritional needs. It’s usually short lived and resolves when the baby feeds more often.
A medical mystery
But GW’s symptoms didn’t resolve. In fact, they got worse: His skin and eyes continued to turn yellow and his stool was a chalky yellow color. Eventually, his doctor ordered a blood test — and when the results came in, Mercedes and Gary knew their instincts had been right. “They said he might need emergency surgery for biliary atresia and told us to bring him to Boston Children’s Hospital for more tests.”
At Boston Children’s, clinicians evaluated GW to try to uncover the reason for his symptoms. While a liver biopsy determined that he didn’t have biliary atresia — the most common cause of chronic liver disease in newborns — it would take more testing before Mercedes and Gary finally had answers.

Not just a liver problem
As GW’s doctors closed in on a diagnosis, the little boy seemed to get sicker: In May 2020, he was admitted to the hospital for a week with what his parents suspected was bronchitis or pneumonia. “We all started to realize that it wasn’t just his liver,” says Mercedes. “Something was up with his immune system, too.”
Working together, hepatologist Dr. Andrew Wehrman in Boston Children’s Center for Childhood Liver Disease, Dr. Sandra Burchett in the Division of Infectious Diseases, immunologist Dr. Craig Platt, and their colleagues ultimately determined that GW had a rare type of immunodeficiency, as well as immune-mediated hepatitis.
Although he may need a bone marrow transplant in the future, for now, GW’s clinicians are able to manage his condition with medication and regular check-ins through virtual visits. “His doctors are amazing,” says Mercedes. “We’ve got a phenomenal care team at Boston Children’s.”

‘Follow your gut’
Treatment seems to be paying off. “His whole personality has changed now that he’s feeling better,” says Mercedes. A typical toddler, GW loves watching Disney’s “Puppy Dog Tales” and is “weirdly obsessed with the refrigerator,” laughs his mom. And he recently became a big brother.
Looking back, Mercedes is glad she and Gary listened to their instincts — and hopes other parents will do the same. “Even though our original doctor thought everything was fine, we knew something was wrong,” she says. “Always follow your gut, do your research, and get a second opinion if you think something isn’t right.”
Learn more about the Center for Childhood Liver Disease
Related Posts :
-

Meghan’s journey with UESL: Finding treatment for a rare form of liver cancer
In the spring of 2017, Meghan Tompkins and her parents, Danni and Michael, arrived at the Dana Farber/Boston Children’s ...
-

A big step toward curbing graft-vs.-host disease after bone marrow transplant
A drug used for rheumatoid arthritis has moved a step closer to FDA approval for a desperately needed new use. ...
-

Going 'all in' for Khori: New hope for congenital enteropathy
Khori LeBlanc is “one of the sassiest and sweetest kids you’ll ever meet,” says her mom, Bryanna Black. Her ...
-

Past patient outcomes could help single-ventricle surgery decisions
When considering whether a child who has a single-ventricle heart defect would benefit more from biventricular repair&...





