How transnasal endoscopy got Jamie back on the golf course

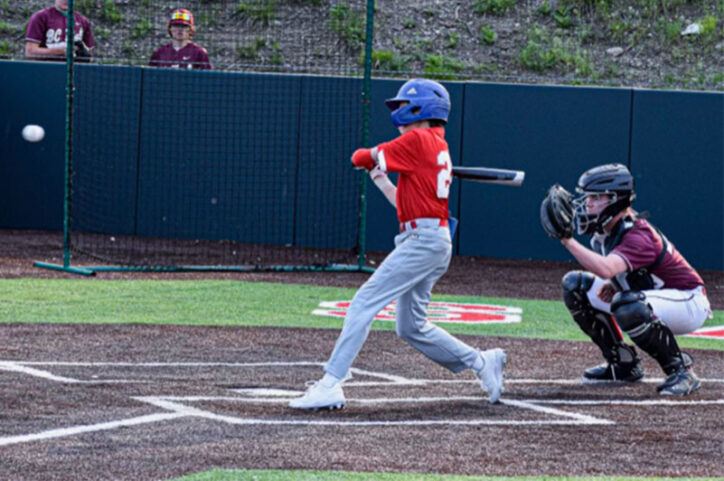
Jamie is like most 15-year-olds — he goes to school, hangs out with his friends, and still makes time to get outside to play some golf and baseball. However, when Jamie was having bouts of throwing up and getting food stuck in his throat, he and his mom, Tricia, knew it wasn’t just a case of a growing teen boy. “I could feel food getting stuck in my throat whenever I ate,” explains Jamie. “I’d run to the bathroom to throw up after coughing so much. It was uncomfortable.”
Jamie and Tricia were already familiar with Boston Children’s Hospital since they live close by, and Jamie was already being seen by Dr. John Lee in the Food Allergy Program for his food allergies. “We told Dr. Lee what was happening with Jamie’s choking episodes,” explains Tricia. “He referred us right away to Dr. Erin Syverson in the Division of Gastroenterology, Hepatology, and Nutrition.”
Finding answers using proven procedures
When they met with Dr. Syverson, she recommended that Jamie have a traditional upper endoscopy to examine his esophagus. In an upper endoscopy, a thin flexible tube with a light at the end is passed through the child’s mouth into the esophagus, stomach, and small intestine. Anesthesia is given to ensure the child is asleep during the procedure. “It was a little nerve-wracking to see your child go through the anesthesia process, but everyone at Boston Children’s was so supportive throughout the entire test,” shares Tricia.
After the endoscopy, Jamie learned that he had eosinophilic esophagitis (EoE), a condition usually related to food allergies in which the lining of the esophagus has become irritated from a buildup of eosinophils, disease-fighting white blood cells.
With the initial endoscopy complete, Jamie and his doctor made a plan to start a medication to treat his EoE and return after a few months for a follow-up endoscopy. However, Jamie and Tricia were given the option to choose between another traditional endoscopy or a newer test called transnasal endoscopy (TNE).
TNE changed the game
Like a traditional endoscopy, a TNE examines the upper gastrointestinal tract by using a thin, flexible tube with a light and a small camera at the end to view the esophagus. What makes this procedure different is that the tube enters through a nostril, rather than the mouth. The test also takes only 5 to 15 minutes and can be performed while awake, without general anesthesia — making a major difference in recovery time and getting back to regular daily routines.
“Dr. Syverson introduced us to Dr. Eitan Rubinstein in the Eosinophilic Gastrointestinal Disease Program to learn more about TNE,” shares Tricia. “Dr. Rubinstein personally called me and talked me through the process, and it sounded like a great alternative to a traditional upper endoscopy.”
For Jamie, it was a no-brainer. “As soon as I heard that the TNE didn’t need anesthesia and I would be able to walk out of the hospital without any assistance, I knew that I wanted to try it out,” Jamie says.
How virtual reality entered the scene
What really made the procedure stand out was the incorporation of virtual reality to distract Jamie while doctors were examining him. “They set me up with the virtual reality goggles and let me watch my favorite golf videos on YouTube,” he smiles. “The whole procedure didn’t hurt at all — I thought it was only five minutes because of how distracted I was, but I guess it was around 15 minutes.”
In total, Jamie and Tricia were at the hospital for around an hour and half — and Jamie was even able to attend his school’s baseball game that afternoon. “For a traditional upper endoscopy, there are a lot more restrictions about what can and can’t be done following the procedure,” explains Tricia. “But TNE got Jamie back to his regular day immediately after, without feeling groggy or sick, and that really made a huge difference to us.”
Next up to plate for Jamie
Jamie’s TNE revealed that his medication was working well, and he would need to take it more often to maintain results. “We’ll need to go back to get a repeat follow-up, but with the initial TNE results we’re feeling really confident about what to look out for and how to keep Jamie healthy,” shares Tricia.
Jamie wants to let other patients with EoE know that if they’re able to get TNE, they’re in good hands. Now, he’s gearing up for summer fun with friends and is looking forward to getting outside to play golf, knowing that his EoE won’t stop him.
To learn more, visit the Eosinophilic Gastrointestinal Disease Program.
Related Posts :
-

Food allergies: Turning tolerance back on
Hans Oettgen, MD, PhD, is Associate Chief of the Division of Allergy and Immunology at Boston Children’s Hospital. He ...
-

Predicting feeding difficulties in children with esophageal atresia: A proactive approach
Children with esophageal atresia are at risk for developing anastomotic strictures, or areas of esophageal narrowing, following surgical repair. Clinicians ...
-

How scratching may prime children with eczema for food allergy and anaphylaxis
Eczema, a chronic itchy inflammatory skin disease, affects about 15 percent of U.S. children. It’s a strong risk factor ...
-

Finding a nutrition plan that works for your family
Every day, millions of people follow specialized diets for myriad reasons. These can include religious or ethical beliefs, allergies or ...