It’s all in the PV loops: New analytical model could improve circulation assessments before heart surgery
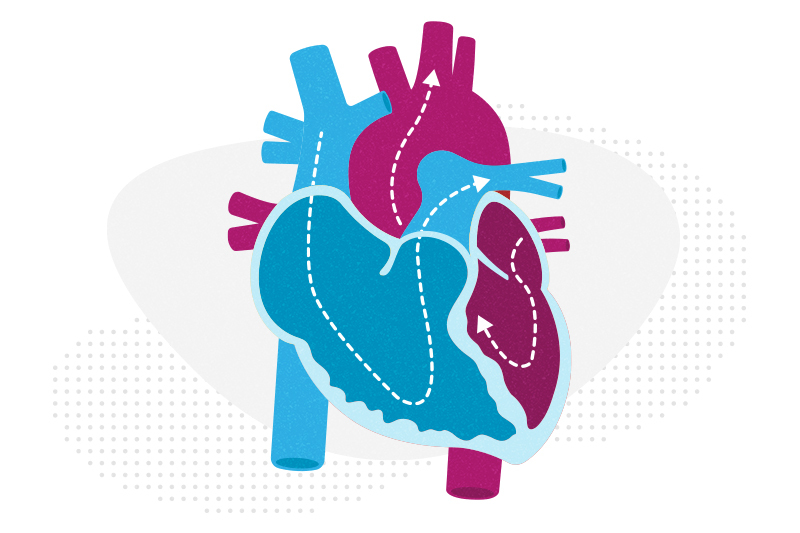
The double-switch operation corrects the congenital reversal of the heart’s ventricles and its two main arteries. It’s a practical way of putting the ventricles into the position they belong so that children with congenitally corrected transposition of the great arteries (CC-TGA) can benefit from enhanced circulation.
Surgery, though, doesn’t come without risks. Some children’s left ventricles — weakened because CC-TGA causes them to pump at a low pressure for too long — are unable to handle an increased workload and fail after an operation. Boston Children’s heart specialists have long wanted to reduce those failures by better understanding the capabilities of a patient’s left ventricle before surgery.
To reach that understanding, cardiologist Nikhil Thatte, MD, has developed an analytical model that draws on ventricular pressure-volume (PV) loop calculations of a changed circulation. The model can help specialists see the strengths and weaknesses of a patient’s ventricle before making a decision on the double-switch operation, he says.
“Children’s hearts come in all shapes and sizes,” says Thatte. “Just knowing what a typical left ventricle looks like doesn’t help you know what each child’s left ventricle needs to do to succeed after a double-switch operation.”
Looking to reverse surgery failure rates
The double-switch operation benefits many children with CC-TGA, but it has a 15 percent failure rate. Some left ventricles can’t handle the workload when they are suddenly introduced to what should have been their normal role of pumping blood throughout the body. The stress can cause severe heart failure. “Although most children do not develop heart failure after the double-switch operation, we have failed if even one child develops this serious complication. We need to do something to reduce that risk,” says cardiologist Rebecca Beroukhim, MD. “But it sometimes can be hard to predict how the left ventricle or heart muscle will behave when you change the circulation.”
Boston Children’s and other hospitals have been trying to decrease the failure rate. But there are no universally accepted standards for assessing the left ventricle in CC-TGA cases. In the meantime, some children who don’t have the operation still experience heart failure because their right ventricle can no longer manage pumping blood to the body.
Assessing the right ventricle gives answers
One day, Thatte had a “lightbulb” idea to solve the problem: Biventricular PV loops could be an ideal predictor of what blood pressure and volume would be after a double-switch procedure. PV loops (two-dimensional graphs that show the relationship between pressure and volume) have been a gold-standard technique to study the mechanical properties of a left ventricle, he says, but they hadn’t previously been used to assess the surgical readiness of a patient’s left ventricle for a double-switch operation. “It gives you as many as 40 indicators of how a ventricle is doing.”
As Thatte studied how PV loops could help, one such indicator — ejection fraction — showed how much blood a left ventricle could eject. But it still couldn’t estimate what the ventricle would be able to achieve after it contracted in the new circulation after surgery. “The load on the ventricle changed a lot from the ‘before’ to the ‘after,’ and that held true for a number of other indicators,” he recalls. “I kept going through different indicators and kept having the same problem.”
Thatte then tried running PV loops on the right ventricle to see if they could provide more insight. They did. Measurements of the right ventricle could estimate what the post-surgery load of the left ventricle would be. “It won’t show the exact load, but I can learn the amount of work required to lift that load, which is what the right ventricle is already doing,” he says. “It’s the best benchmark I can compare against, which is the other half of the patient’s own heart.”
A formula that previews a new circulation
Incorporating both ventricles helped Thatte arrive at an assessment formula that was shaped by two approaches. The first approach reviewed pressure volume area metrics that a conductance catheter had collected from the left ventricles of 20 patients. But because not every heart center has a conductance catheter, Thatte tried a second approach. He found that the same metrics could also be captured by a regular catheter and MRIs. Using those common tools can help all levels of hospitals assess patients for double-switch operations.
Both approaches established a strong relationship between the measurements and estimations of three key ventricular benchmarks: work to eject blood (stroke work), potential energy of contraction, and their sum: the total pressure volume area. “We established the relationship between what the conductance catheter was giving and what the simple variables of the MRI and catheter were giving, and that’s the formula we came up with,” Thatte says.
Thatte, Beroukhim, Sunil Ghelani, MD, and others then looked to see if the formula (LV:RV ePVA ratio >0.67) would have accurately predicted the outcomes of 42 double-switch operations performed at Boston Children’s. “It did a really good job of predicting how those patients did,” Thatte says. They are now preparing a research paper to detail those and other findings. They also want to create an open-source calculator that specialists could use to input the measurements and calculations of patients’ ventricular circulations. Those numbers can be gathered from either a conductance catheter or a regular catheter and MRI scans.
Another approach to circulation assessment
Thatte, Ghelani, and other researchers further validated biventricular pressure-volume loop analysis in another study using a computational modeling approach on the datasets of six patients. It provided nearly identical results as their review of the 42 patient outcomes, despite using a very different methodology.
Calculating the effectiveness of ‘training’
If a child with CC-TGA isn’t ready for a double-switch operation, Boston Children’s heart specialists will, if possible, strengthen their left ventricle through “training.” They surgically place a band on the pulmonary artery to create a higher pressure load on the ventricle and prepare it for the eventual change of circulation. Sometimes they will also create a hole between the upper two chambers of the heart (the atria) to increase blood flow.
The new PVA formula developed by Thatte helps determine if those methods have worked and if a child is ready for the double-switch operation. “It lets us see if a child is at their best state before having the surgery, or if should we do more to prepare them better.”
Learn more about the Complex Biventricular Repair Program.
Related Posts :
-

A 'super' new heart surgery for a super kid
When you’re the first person in the world to undergo a new type of heart surgery, you don’t ...
-

After four unsuccessful heart surgeries, Nicholas finds hope
When Brenna and Lorenzo Degano arrived in Boston with their son, Nicholas, last April, it was with a feeling of ...
-

From aerospace to the OR: 3D modeling improves surgical planning by revealing details of patients' hearts
One of the most important tools for complex heart surgeries at Boston Children’s isn’t even in the operating ...
-

Conduction tissue mapping is shown to significantly reduce heart block
New research by Boston Children’s validates an innovative approach to mapping the heart’s invisible conduction tissue during surgery. ...





