Poverty predicts worse cancer outcomes, even in children receiving top-tier care

A pair of recent studies suggests that even among patients receiving advanced cancer care, poverty is a predictor of worse outcomes. The disturbing findings raise many questions that follow-up studies are now exploring.
Key takeaways
- Poverty was associated with 3.7-fold higher mortality among children receiving targeted immunotherapy for high-risk neuroblastoma.
- Household poverty was associated with 28 percent higher mortality from transplant complications and 23 percent higher overall mortality among children receiving donor stem cell transplants for various cancers.
The studies were led by Kira Bona, MD, MPH, of the Dana-Farber/Boston Children’s Cancer and Blood Disorders Center. They reviewed outcomes among children receiving targeted therapies for high-risk neuroblastoma, the most common tumor in young children, and among children receiving blood stem cell transplants for cancer or various blood disorders.
Both studies used two measures of poverty: neighborhood poverty (living in low-income zip codes) and household poverty (having public health insurance like Medicaid).
“Nearly one in five U.S. children live in poverty,” Bona says. “This is a significant opportunity to improve childhood cancer outcomes.”
Could poverty negate the progress made with new cancer therapies?
The neuroblastoma study reviewed the outcomes of 371 U.S. children with high-risk neuroblastoma. All received targeted immunotherapy at specialized cancer centers through randomized clinical trials sponsored by the Children’s Oncology Group. This highly effective treatment has produced the greatest gain in neuroblastoma survival in decades.

“Our question was, does access to the best cancer care we know how to provide, in state-of-the art clinical trials, prevent disparities in outcome?” says Bona. “The answer seems to be no.”
While neighborhood poverty did not independently predict cancer relapse or mortality, children exposed to both household and neighborhood poverty had 2.2-fold worse event-free survival and 3.7-fold higher mortality than children not exposed to poverty. (The researchers defined events as relapse, progressive disease, or secondary malignancy.)
In simple terms, two years after treatment, event-free survival was 22 percentage points lower for children exposed to both measures of poverty than for children not exposed to poverty (55 vs. 77 percent). Overall survival was 26 percentage points lower (64 vs. 90 percent).
Findings were published today in the Journal of the National Cancer Institute (JNCI).
Poverty and stem cell transplant outcomes in children with cancer
The second study, published October 26 in the journal Blood, tapped the largest national database of pediatric stem cell transplant outcomes, maintained by the Center for International Blood and Marrow Transplant Research (CIBMTR).
Seeing children disproportionately dying because they are exposed to poverty is unacceptable.”
– Kira Bona
Bona and her colleagues looked at outcomes in children who received a first-time donor stem cell transplant. Of these children, 2,053 had cancer (acute leukemias, chronic myeloid leukemia, and lymphomas) and 1,696 had non-malignant disease. (These were blood disorders including sickle cell disease, severe aplastic anemia, severe combined immunodeficiencies, inherited disorders of metabolism, and histiocytic disorders).
The team adjusted the data for multiple factors, including age, ethnicity, disease status, closeness of donor match, and intensity of the pre-transplant conditioning regimens.
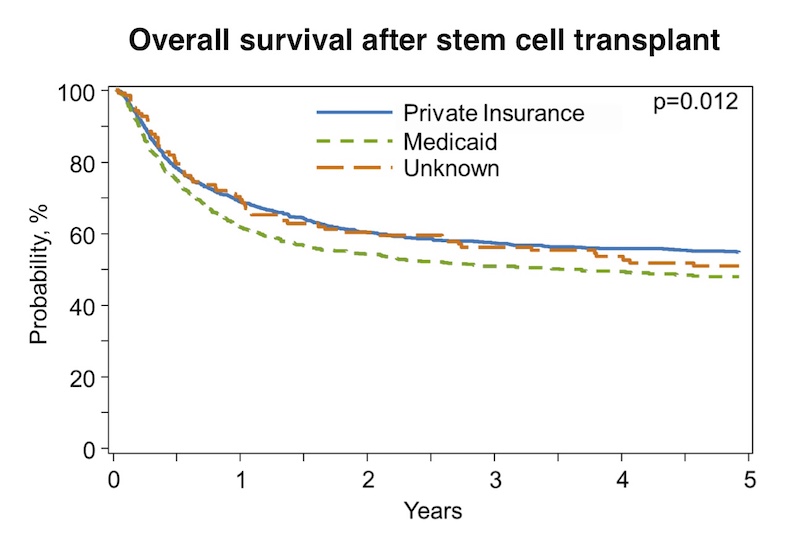
Among the children receiving transplants for non-malignant disease, poverty was not predictive of survival. But among the children with cancer, those who were exposed to household poverty had 28 percent higher mortality from transplant complications and 23 percent higher overall mortality than children not exposed to poverty. Those exposed to neighborhood poverty had a 34 percent increase in transplant-related mortality, but they had no difference in overall survival.
While the study did not set out to look at race, it found a striking disparity. Black children with cancer had a 47 percent higher risk of death overall and a 65 percent higher risk of transplant-related mortality than white children.
“This definitely deserves further investigation in a dedicated fashion,” says Bona.
Exploring social determinants of health
Why did poverty so often predict worse outcomes? In the case of neuroblastoma immunotherapy, Bona believes that poverty may affect children’s underlying ability to respond to the treatment, as well as their ability to access care once they leave the controlled hospital setting.
“We know that children living in poverty are more likely to experience stress and to have comorbid illnesses and poorer health, so they may be more likely to experience toxicity from their treatment that could result in treatment delays or complications,” she says.
“Also, we saw a bigger difference in survival than in relapse. This raises the question of whether these children were less able to access effective relapse therapies after leaving the immunotherapy trial. These therapies are often available only at select hospitals and may require significant travel and parents’ time off from work.”

In the stem cell transplant study, Bona suspects the greater mortality associated with poverty among children with cancer may reflect their access to post-transplant care.
“These children accessed a highly complex tertiary procedure, but once they completed the transplant and went home, they might have had decreased access to care,” she says. “We need to investigate that.”
Why was poverty not a factor for the children with non-malignant disease? Bona notes that there are treatment options for non-malignant disease other than transplant, unlike for cancer.
“Transplant may have been preferentially offered or chosen by families preferentially when the child had more social resources, even if they were exposed to poverty,” she says. “That could have resulted in a cohort of children who were better able to survive the rigors of transplant.”
Baking poverty and social factors into clinical studies
The studies have sparked further research to explore the role of poverty in cancer outcomes. One study, using banked tumor samples, is exploring the possibility that children exposed to poverty may have changes in their cancer cells or immune system that might affect their response to immunotherapy. But Bona also wants to see poverty measures explicitly included in clinical studies.
If our goal is to cure every child, ensuring access to novel therapies is simply not enough.”
– Kira Bona
She and her colleagues are directly surveying families participating in clinical trials sponsored by COG and the Dana-Farber Cancer Institute about food, housing, transportation, and utility insecurity. A separate study, the first of its kind, is exploring the feasibility of providing families with food and transportation during treatment in hopes of improving cancer outcomes. Early results published in the journal Pediatric Blood Cancer are highly promising.
As for stem cell transplant, Bona is working with the CIBMTR to add parent-reported measures of poverty to its database.
“Seeing children disproportionately dying because they are exposed to poverty is unacceptable,” says Bona. “If our goal is to cure every child, ensuring access to novel therapies is simply not enough. We have to integrate social determinants of health into every clinical trial that we run and actively consider them as potential risk factors that we can target with interventions.”
Visit the Bona Lab to learn more about its health equity research, and read more stories related to social determinants of health.
Related Posts :
-

A new druggable cancer target: RNA-binding proteins on the cell surface
In 2021, research led by Ryan Flynn, MD, PhD, and his mentor, Nobel laureate Carolyn Bertozzi, PhD, opened a new chapter ...
-

Forecasting the future for childhood cancer survivors
Children are much more likely to survive cancer today than 50 years ago. Unfortunately, as adults, many of them develop cardiovascular ...
-

Pediatric high-grade gliomas: Research reveals effective targeting with avapritinib
Pediatric high-grade gliomas, particularly H3K27M diffuse midline gliomas (DMG), are aggressive malignant brain tumors with a poor prognosis. ...
-

Blood across our lifetimes: An age-specific ‘atlas’ tells a dynamic story
The stem cells that form our blood, also known as hematopoietic stem cells (HSCs), are with us throughout our lives. ...





