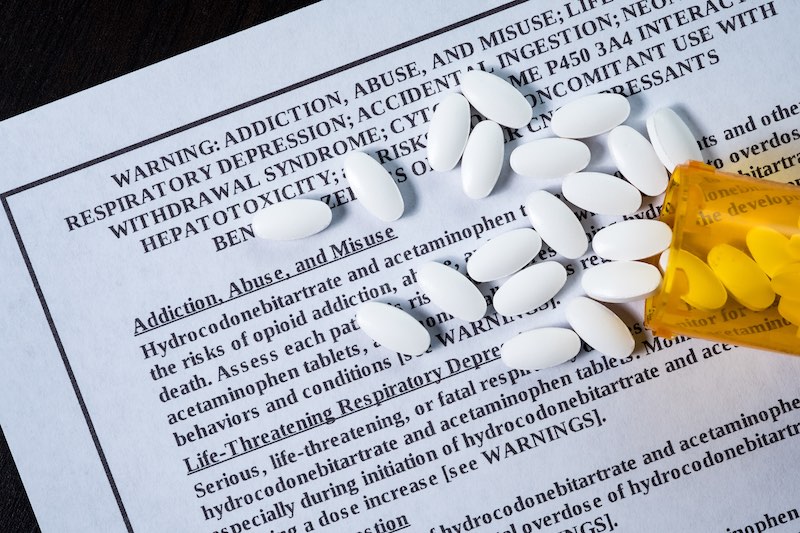
Concerning rates of opioid prescribing to teens and youth

Teens and young adults are notably susceptible to misusing opioids and becoming addicted once exposed. Opioids should be used with great care in this group. Yet a large national study from Boston Children’s Hospital finds that opioid prescriptions to youth aged 13-22 are much like those in older adults.
Based on 2005-2015 data from the National Hospital Ambulatory Medical Care Survey and the National Ambulatory Medical Care Survey, the most recent data available, nearly 57 million youth visits to emergency departments or outpatient clinics involved an opioid prescription. That included 15 percent of ED and 2.9 percent of outpatient visits. Hydrocodone was the most common drug prescribed.
The findings were published today in the journal Pediatrics.
“It’s concerning that we’re continuing to prescribe opioids at these rates to this high-risk population,” says Joel D. Hudgins, MD, of Boston Children’s Hospital’s Division of Emergency Medicine, the study’s first author. “There are more risk-taking behaviors among teens and young adults and increased susceptibility to behaviors that can lead to substance abuse and addiction.”
Opioid prescriptions to youth in the ED
The highest overall rate of opioid prescribing — 18 percent of visits — was for young adults age 18–22 visiting the emergency department. Prescribing rates in the ED were greatest for dental disorders (60 percent of adolescent and 58 percent of young adult visits) and for orthopedic injuries in adolescents (clavicle fractures, 47 percent; ankle fractures, 38 percent).
Other notable, possibly questionable indications in the ED included abdominal pain in young adults (with 20 percent of visits involving opioids), ankle sprains in adolescents (16 percent), urinary tract infection in young adults (17 percent), and headache (8 percent of adolescents, 19 percent of young adults). Young adults with low back pain were prescribed an opioid 38 percent of the time.
“These data give us the opportunity to highlight specific prescribing patterns and treatment norms that may need to be adjusted,” says Florence T. Bourgeois, MD, MPH, of Boston Children’s Division of Emergency Medicine and Computational Health Informatics Program (CHIP), who was the study’s senior author. “It’s been a reflex for clinicians in certain specialties to prescribe opioids, and we need to change those approaches. For many of these conditions, there is evidence that Tylenol or Motrin may work just as well in managing pain.”
Opioid prescribing to youth in outpatient clinics
For all ages, outpatient visits were most likely to involve an opioid prescription in general surgery clinics (9 percent of visits), orthopedic surgery clinics (8 percent), clinics classified as “other specialties” (e.g. gastroenterology, hematology, vascular medicine; 7 percent), and family practice clinics (4 percent).
The lowest rates of opioid prescribing were in psychiatry clinics (1 percent of visits), pediatric clinics (0.4 percent), and ob/gyn clinics (2 percent).
The study also found geographic differences that seem to speak to local medical practice. For example, rates of opioid prescribing to youth in the ED were lowest in the Northeast (10 percent of visits) and highest in the West (18 percent).
Unfortunately, the investigators did not have information on prescription duration, quantity of opioids dispensed, or how well patients adhered to prescription instructions.
Are opioid prescribing patterns changing?
The study was limited by data being available only through 2015, a time when opioid addiction was entering broad public awareness.
When Bourgeois and colleagues looked over the 10-year period, the rate of opioid prescribing nationally fell off slightly in the ED, but not in outpatient clinics.

Hudgins sees hope in the most recent data, which show a dip in 2015. Has public attention finally started to change practice? Only time will tell. Hudgins and Bourgeois look forward to analyzing additional years of data when they’re released.
“The 10-year trend indicates that over-prescribing of opioids most likely remains a substantial problem,” Bourgeois says. “I think we’ve been starting to move the needle a little bit, but additional interventions and education are needed.”
Coauthors on the paper were John J. Porter, MBA, and Michael C. Monuteaux, ScD, also of Boston Children’s. The work was supported by a grant from the Burroughs Wellcome Fund.
Related Posts :
-

Parsing the promise of inosine for neurogenic bladder
Spinal cord damage — whether from traumatic injury or conditions such as spina bifida — can have a profound impact on bladder ...
-

Which pain medication is right for your child? What a pediatrician wants parents to know
There’s no shortage of safe and effective pain medications for children. Acetaminophen (commonly known as Tylenol), ibuprofen (Motrin, Advil), ...
-

Unveiling the hidden impact of moyamoya disease: Brain injury without symptoms
Moyamoya disease — a rare, progressive condition that narrows the brain’s blood vessels — leads to an increased risk of stroke ...
-

Forecasting the future for childhood cancer survivors
Children are much more likely to survive cancer today than 50 years ago. Unfortunately, as adults, many of them develop cardiovascular ...