Conduction tissue mapping is shown to significantly reduce heart block

New research by Boston Children’s validates an innovative approach to mapping the heart’s invisible conduction tissue during surgery.
Key takeaways
- Using a catheter to map unseen conduction tissue drastically reduces heart block during biventricular repair surgeries for several heart conditions.
- Conduction tissue was identified in 96 percent of patients who were mapped.
- Only 4 of 25 patients who were mapped for a ventricle septation procedure experienced heart block that required a permanent pacemaker.
Research data from separate studies show that using electrophysiology tools to avoid the inadvertent injury of unseeable conduction tissue has drastically reduced postoperative heart block — and the need for a pacemaker — in the treatment of several congenital heart defects (CHDs).
“It’s incredibly gratifying we were able to show that this does make a difference,” says cardiologist Elizabeth DeWitt, MD, principal investigator of the larger of the two studies. “Cardiologists get involved at the outset to prevent heart block and pacemakers from happening — and then the cardiac surgeons can make these amazing repairs.”
Surgeries for several conditions benefitted
A few years ago, DeWitt teamed up with fellow cardiologist Edward O’Leary, MD, and cardiac surgeon Eric Feins, MD, to find a way to “see” conduction tissue that is invisible to the naked eye. They started using a catheter for intraoperative conduction tissue mapping, guiding surgeries that treat heterotaxy, transposition of the great arteries, atrioventricular canal defects, and ventricular septal defects (VSDs). This year, they finally had enough data to compare heart surgeries that included conduction mapping and those that didn’t.
As they recently highlighted in the Journal of the American College of Cardiology, conduction mapping significantly reduced postoperative heart block and the need for pacemaker implantation in patients who underwent complex biventricular (BIV) repair to treat several types of CHD. The study compared 149 patients who had conduction mapping, from 2019 to 2022, with 201 patients whose surgeries weren’t mapped, from 2013 to 2021. (Conduction tissue was identified in 144 of those 149 mapped patients.)
The breakdown of patients who experienced heart block and needed a pacemaker after procedures that were mapped and unmapped was:
- Heterotaxy: 2 percent of those who were mapped and 16 percent who weren’t
- Without L-malposition of the great arteries: 3 percent mapped and 11 percent unmapped
- VSD enlargement: 9 percent mapped and 22 percent unmapped
“There are certain high-risk patients who are mapped but are still developing heart block at the same rate as those without mapping, so more needs to be done to help them,” says O’Leary, who was a study co-lead author with Feins. “But the data show we’ve identified several groups of conditions where there was a meaningful reduction in heart block and a need for a permanent pacemaker. Those patients can benefit from mapping.”
Promising results in study of ventricular septation
One group of patients that is benefitting is children who have double-inlet ventricle (DIV). Sitaram Emani, MD, another of the larger study’s authors, was principal investigator of a separate study that looked at mapping results from ventricular septation procedures to treat DIV. Published recently in the Journal of Thoracic and Cardiovascular Surgery, this study found that only 4 of 25 patients who were mapped during the procedure experienced heart block that required a permanent pacemaker.
This was a promising finding because ventricular septation is a favored alternative to the Fontan procedure. (The Fontan treats single-ventricle heart defects but it can have complications for some children.) Patients with DIV have complex heart anatomies that make it difficult to pinpoint conduction tissue. “But with mapping, you can reduce heart block down to about 10 percent, and that makes a big difference,” Emani says.
“It means we can move forward on ventricular septation with confidence. Many children who have the procedure are doing quite well and have been able to avoid the Fontan, which is a goal.”

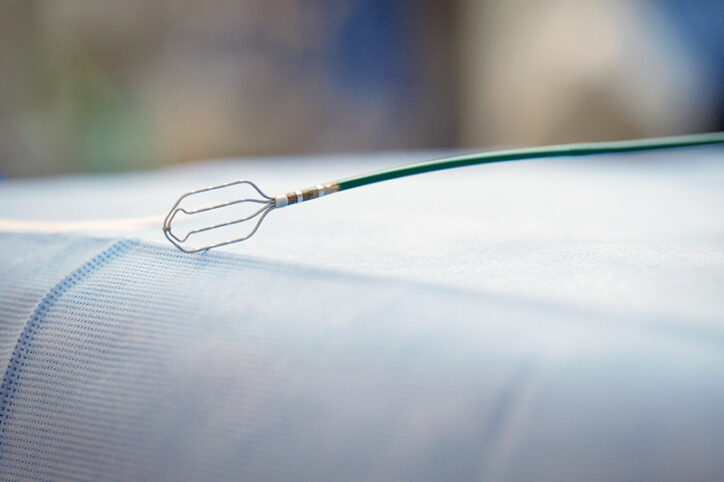
Using the research to improve outcomes
Work to improve conduction tissue mapping continues. For one, the team wants to someday put aside the catheter that was repurposed to find conduction tissue (it’s meant to treat arrhythmia). They’d prefer to use a tool that’s specifically developed for mapping during surgery. Jocelyn Davee, a medical device research engineer, is testing prototypes. Meanwhile, the heart specialists will closely review why mapping works well for certain conditions and not others.
“It’s critical that we don’t rest on our laurels,” Feins says. “We have this mostly figured out, but we need to keep getting more patients mapped and constantly push to make it better.”
Learn more about the Surgical Electrophysiology Program and Electrophysiology Service, or refer a patient.
Related Posts :
-

Finding ways to reduce the financial and social costs of pacemakers
As the number of complex heart operations has increased over the years, so have cases of postoperative heart block, a ...
-

Two new approaches to identifying conduction tissue
Conduction cells in the heart are responsible for initiating contraction of the heart muscle. The inability to properly identify the ...
-

"Seeing" the unseen: A way to pinpoint elusive cardiac conduction tissue
When patients with congenital heart issues have an operation, surgeons have to proceed with an “eye of faith” as they ...
-

A new lens on cardiac surgery could help prevent arrhythmia
Sometimes, a change in perspective can lead to a medical breakthrough. A type of microscopy typically used to detect cancer ...