New study ties residual lesion score (RLS) to cardiac surgery outcomes

How well a patient does after surgery for congenital heart disease (CHD) depends on a large number of variables, ranging from patient characteristics to preoperative status to anatomic complexity to perioperative factors. One of the most important predictors of adverse events or reintervention is the presence of residual lesions — structural cardiac abnormalities that remain postoperatively, whether intended or not.
To further understand the correlation between residual lesions and patient outcomes, a group of clinicians at Boston Children’s Hospital developed a novel quality improvement tool, called the residual lesion score (RLS), and tested its validity in a prospective multicenter study published in 2019.
“As heart surgeons, we know that leaving behind a residual lesion does affect a patient’s outcome, but there was no definitive way to measure the severity of the residual lesion and to prospectively follow patients and measure what happens,” says Meena Nathan, MD, MPH, cardiac surgeon at Boston Children’s and first author on the paper. “The nature of heart surgery is such that there are some procedures where it may not be possible to perform the intended repair because of the anatomic complexity of the heart defect or other characteristics, so we wanted to know what is an acceptable result, and how that might affect a patient over time. That’s why we developed this score. ”
Determining residual lesion score
The RLS classifies residual lesions into three categories: RLS 1, meaning trivial or no residual lesions; RLS 2, minor residual lesions; or RLS 3, major residual lesions or unplanned reintervention for such lesions before discharge.
“Because there are so many different variations of the same operation in heart surgery, we developed modules for each component of each operation to create a score depending on what was done,” says Nathan. “Then we assigned the score based on echocardiographic and clinical findings at the time of discharge and followed the patients to see how they did.”
New study builds on findings
Building on those findings, a new multicenter observational study, published in the May 2021 issue of the Journal of the American College of Cardiology, prospectively explores the impact of the severity of residual lesions on postoperative outcomes across operations of varying complexity.
The study enrolled 1,149 infants in 17 sites who were undergoing one of five common congenital cardiac operations of increasing complexity: tetralogy of Fallot (TOF) with pulmonary stenosis repair, complete atrioventricular septal defect (CAVSD) repair, arterial switch operation with or without ventricular septal defect (VSD) closure, coarctation/hypoplastic or interrupted arch with VSD closure (Arch/VSD), or the Norwood operation.
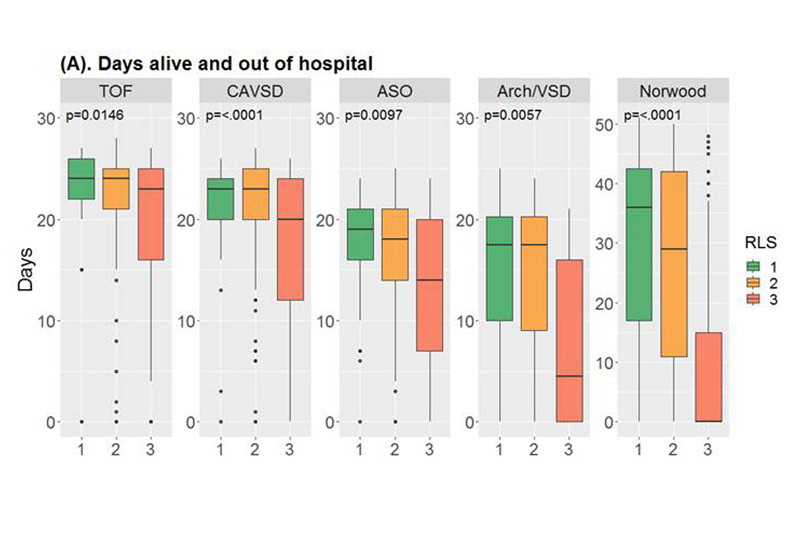
The primary outcome was defined as number of days alive and out of hospital within 30 days after surgery (60 days for Norwood). Secondary outcomes included total postoperative hospital length of stay, initial and total postoperative duration of mechanical ventilation, initial and total length of postoperative intensive care unit (ICU) stay, and incidence of major postoperative events.
The study found that patients with major residual lesions (RLS 3) fared worse on both primary and secondary outcomes across all operations, with fewer days alive and out of the hospital at 30 days (60 for Norwood) and a longer hospital length of stay. This was true even after controlling for patient and preoperative factors. For the two most complex operations, the Arch/VSD and Norwood, the researchers found that major residual lesions were significantly associated with worse outcomes, which included duration of mechanical ventilation, ICU stay, and major medical events. Primary and secondary outcomes did not differ consistently between RLS 1 and 2.
Clinical learnings from RLS
“This score helps identify a group of patients who need closer follow-up upon discharge,” says Nathan. “It also helps surgeons understand which of the congenital cardiac operations may need further refinement, so it serves as a self-assessment tool.”
Nathan says that since the RLS was developed, surgeons at Boston Children’s have used a patient’s projected RLS score after surgery to inform surgical decisions.
“If a surgeon sees that a residual lesion score for a given operation is going to be between 2 and 3, we will often take the patient immediately back to surgery to see if there’s a way to fix the issue to help them do better over the long term,” says Nathan. She is currently analyzing data to see how well such patients fare compared to those who did not have a planned reintervention before discharge.
“This is the first study to evaluate RLS across several institutions,” says Nathan. “We believe it can serve as an instrument to guide perioperative strategies to improve outcomes of congenital heart surgery for patients.”
Looking ahead, Nathan is continuing to fine-tune the tool, including finding a way to measure RLS earlier in the process, before hospital discharge, to help further improve patient outcomes.
Learn more about the Department of Cardiac Surgery.
Related Posts :
-

A complex repair for Ruby’s heart
When Rebecca and Michael Stewart learned their baby would be born with a congenital heart condition, they reacted as any ...
-

A repair for Charleston’s complex heart
Trey and Jandie Steele both work in medical device sales. They have spent lots of time in hospital operating rooms ...
-

Heart strong: Two families bond over shared challenges
Four years ago, Ali Marcus walked through the door of a coffee shop in Connecticut and met the woman who ...
-

Parsing the promise of inosine for neurogenic bladder
Spinal cord damage — whether from traumatic injury or conditions such as spina bifida — can have a profound impact on bladder ...





