Finding ways to reduce the financial and social costs of pacemakers
As the number of complex heart operations has increased over the years, so have cases of postoperative heart block, a form of arrhythmia that often requires a pacemaker and more surgery. Heart block occurs when unseen conduction tissue — the cells and electrical signals that control the beating of a heart — is injured.
It is a complication that’s universal to all hospitals, and it is why Boston Children’s has dedicated resources toward reducing heart block, improving health care costs for families, and enhancing young patients’ quality of life.
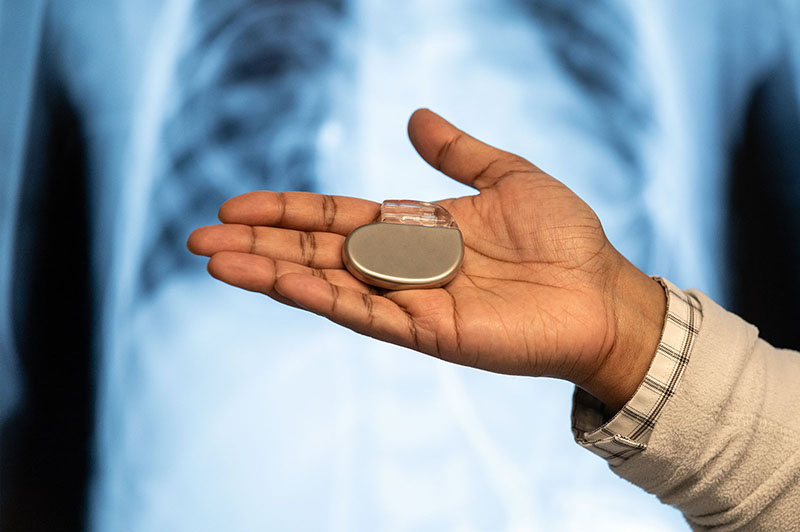
“Children who have pacemakers tell us their concerns about these devices. The idea of a machine controlling their hearts gives them doubts,” says Douglas Mah, MD, director of Boston Children’s Pacemaker and ICD Program.
Aiming to reduce the need for pacemakers, Boston Children’s clinicians have created two new approaches to cardiac surgery that can identify elusive conduction tissue and potentially decrease heart block. The innovations have already shown promise. “We have to prevent heart block,” says Aditya (AK) Kaza, MD, a Benderson Family Heart Center cardiac surgeon. “We can’t just dismiss it and say there’s always going to be a percentage of patients who will need pacemakers. We have to get that number to the absolute minimum.”
Pacemakers can put a strain on families
Aside from causing anxiety in children, pacemakers can be costly. But no one had ever looked at the economic impact on families, prompting Kaza, Mah, and other Boston Children’s researchers to look at those costs.
Reviewing Boston Children’s medical records of congenital heart disease surgeries from 1960 to 2018, they found that 968 out of 28,225 pediatric patients needed a pacemaker because of postoperative heart block. Two other statistics illustrate how heart block has been related to the increasing complexity of heart surgery: As the number of operations increased by 2.2 percent per year, the number of pacemaker implantations climbed by 7.2 percent per year.

The study, which was led by Abhijit Mondal, PhD, and published in JAMA Network Open, also found that over a 20-year span, the direct and indirect costs of pacemaker implementation and management were nearly $200,000. For families of pacemaker patients who were younger than 4, direct costs — including implantation surgery, replacements, and follow-up care — averaged $180,664, while indirect costs from hospital visits — hotel, gas, and meals — averaged $15,939.
“It’s a huge burden,” says Kaza, who was the principal investigator of the study. “But the financial burden is only a small part of what families experience. There is also the impact of a pacemaker on heart health and the general health of a child.”
Children can be stressed by a pacemaker
Although it’s uncommon, pacemakers can malfunction and cause complications, Mah says. Also, batteries, which last as long as 15 years, will eventually need to be replaced, usually through a medical procedure. But even if a pacemaker functions properly over long stretches, children can’t avoid seeing it on their chest and recognizing they depend on a device to keep their heart functioning.
“There’s growing knowledge that many children who have pacemakers can have undiagnosed anxiety,” says Mah, pointing to research by Boston Children’s. “Not only does a family have a financial burden, but they also might have an anxious child.”
The recent financial study, though, gives Mah, Kaza, and their colleagues an opportunity to shine a light on two Boston Children’s initiatives that look to help children by preventing heart block in the first place.
Configuring a microscope to find conduction tissue
Conduction tissue is invisible to the naked eye and imaging technologies in operating rooms. Heart surgeons say they instead rely on an “eye of faith.” Kaza and his research team have found a different type of “eye” — a confocal microscope the size and shape of a bendable straw. Fitting comfortably in a surgeon’s hands, the microscope offers a high-resolution view of tissue by blocking out-of-focus light to create a perspective that helps pinpoint the spot of the tissue.
A confocal microscope looks closely at heart muscle cells
Learn how a confocal microscope helps cardiac surgeons. Click Here
The microscope looks about 50 millionths of a meter below the heart’s surface, or about half the thickness of a standard sheet of notebook paper. It doesn’t reveal conduction tissue itself but instead illustrates the visual differences between heart muscle cells and conduction tissue regions. When surgeons look at the different presentations of heart muscle cells, they will recognize areas that are known to have conduction tissue and will mark those spots to avoid them.
Kaza’s team continues to test the confocal microscope. In 2022, Kaza and other Boston Children’s cardiac surgeons published a study in the Annals of Thoracic Surgery detailing how the microscope assisted in the operations of 27 patients; the technology has since been used in 43 more operations. Preliminary analysis revealed substantial differences in the location of conduction tissue in hearts with ventricular septal defects, tetralogy of Fallot, and atrioventricular canal defects.
An EP tool guides cardiologists toward conduction tissue
On another track, Boston Children’s cardiac surgeons, cardiologists, and engineers are testing the use of an electrophysiology (EP) tool to find conduction tissue in hearts beating naturally during surgery. The team found that the tool — a grid-mapping catheter often used by electrophysiologists to treat arrhythmias — could quickly and accurately pinpoint conduction tissue during an operation.
How does conduction tissue mapping work?
Watch Boston Children’s heart surgeon Eric Feins explain how conduction tissue mapping works and how it has reduced postoperative heart block. Click Here
The tool collects electrical signals that an electrophysiologist reads out in real time, helping surgeons determine where conduction tissue runs. “It allows for very quick identification and communication, from the signals that we see on the screen to what the surgeons are seeing in the operating field,” says cardiologist Edward O’Leary, MD, who is working on the initiative with fellow cardiologist Elizabeth DeWitt, MD, and cardiac surgeon Eric Feins, MD.
The EP tool has aided more than 350 surgeries at Boston Children’s and prevented heart block in many patients — especially those with heterotaxy who need complex biventricular repair. In that patient group, the rate of heart block has decreased from over 14 percent to less than 3 percent when conduction mapping is performed during surgery, Feins says.
Aiming to help children overcome psychological hurdles
Even if incidents of postoperative heart block drastically decrease, some children will still need a pacemaker. Hospitals should remain committed to giving them high-quality care during implantation, device maintenance, and all other steps of their journeys, Mah and Kaza say. Children should also have access to social and psychological resources.

“Children worry about having to talk to airport security agents about setting off metal detectors,” Mah says. “They worry about what happens if the pacemaker gets hit during baseball, taekwondo, and other activities. We tell them it’s okay, but it’s hard to completely reassure them.”
That’s why the two innovations are important, Kaza says. “We’re saying we don’t have to accept the idea that everybody needs a pacemaker.”
Learn more about the Benderson Family Heart Center or refer a patient.
Related Posts :
-

From aerospace to the OR: 3D modeling improves surgical planning by revealing details of patients' hearts
One of the most important tools for complex heart surgeries at Boston Children’s isn’t even in the operating ...
-

Finding a way to help newborns who can't immediately have heart treatment
Newborns with complex congenital heart defects (CHD) and pulmonary overcirculation often need treatment as soon as possible. Unfortunately, ...
-

Experience and innovation create a safer type of heart surgery
The Eureka moment came the day before heart surgery. Easton Schlein wasn’t an ideal candidate for a full-scale surgical ...
-

The secret to safer heart surgery lies in modernizing an old technique
Of the many features in the recently-opened Hale Family Building at Boston Children’s, maybe one of the ...