Finding a way to help newborns who can’t immediately have heart treatment
Newborns with complex congenital heart defects (CHD) and pulmonary overcirculation often need treatment as soon as possible. Unfortunately, some of these children are not in good enough health to withstand surgery.
To address this challenge, Boston Children’s heart specialists leaned into technological innovation, their experience, and a perseverance that would ultimately confirm their belief that even the highest-risk cases are not out of reach.
Other heart clinicians will recognize the innovation as the reconfiguration of a vascular plug to act as a pulmonary artery (PA) flow restrictor — making Boston Children’s among the first U.S. hospitals to use the specific technology as a palliative measure for newborns with CHD and overcirculation. But for parents of newborns with serious heart conditions that can’t be immediately treated, the innovation simply means there’s a new way to help prepare their children for surgery.
“It could be a game changer,” says Nicola Maschietto, MD, PhD, a cardiologist at Boston Children’s Benderson Family Heart Center. “We are possibly on the verge of a shift in how we care for these critically ill newborns.”
Finding and refining a device that could help
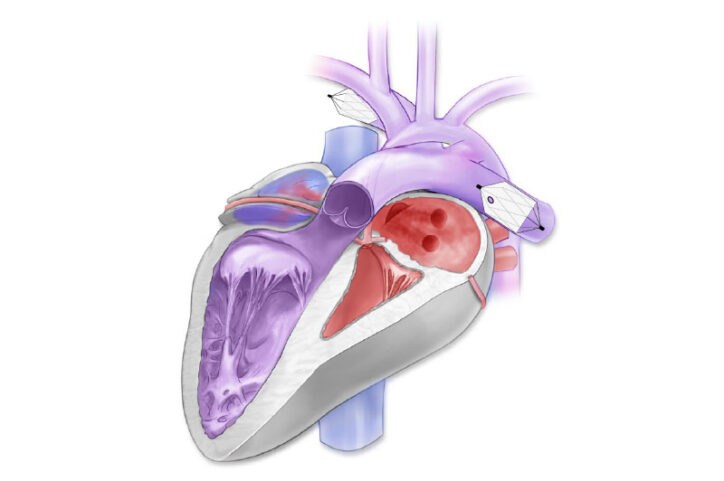
A newborn with complex CHD such as a single ventricle defect already faces a significant challenge: An underdeveloped ventricle can’t effectively pump blood, leaving the bulk of work to the other ventricle. But when a newborn also has overcirculation (too much blood delivered to the lungs’ arteries), the healthy ventricle struggles to handle blood flow, potentially damaging an already compromised heart. These patients, especially those born prematurely, are weak and would face risks if they had immediate treatment.
What is embolization?
It is a minimally invasive, image-guided treatment that injects a special material or device into a blood vessel to block or close it.
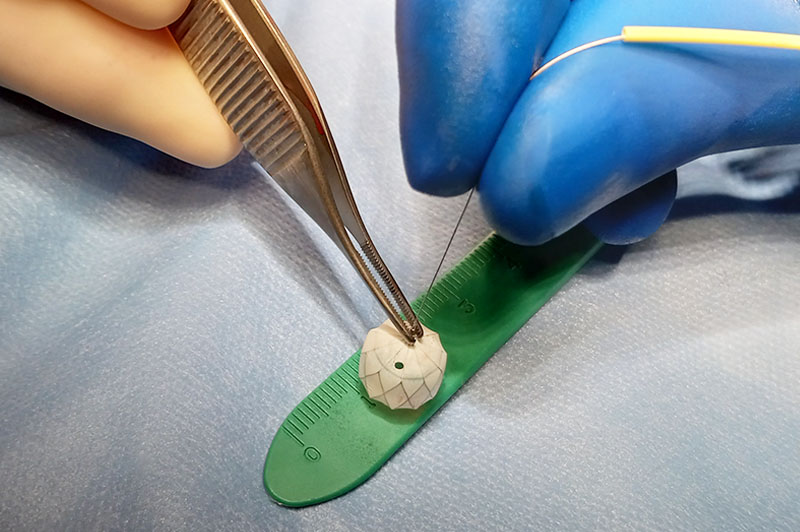
In late 2021, a child born prematurely had a single ventricle anatomy and overcirculation. He barely weighed three pounds. Unable to apply any standard treatment option, Maschietto and cardiac surgeon Christopher Baird, MD, wanted to slow the child’s blood flow to the lungs until his health and weight reached a stage where he could have surgical repair. Cardiologists attempt to limit blood flow in patients through a cardiac catheterization, but most implanted devices are too large to work effectively in newborns. A commercially-available vascular plug for treating serious bleeding seemed to be a solution. It was just the right size for the newborn’s pulmonary arteries, but there was one catch: It was designed to completely block blood flow in a vessel.
Still, Maschietto and Baird saw its potential and reconfigured the device by creating a tiny opening on its top, allowing a small amount of blood to reach the lungs and limiting blood pressure. They implanted a device in each of the child’s pulmonary artery branches through a microcatheter and watched with excitement over the next few months as he became healthy enough for surgical repair.
Testing opens the door to widespread use
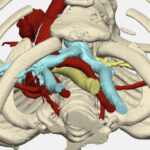
The child’s recovery encouraged Maschietto and Baird to refine their PA flow restrictor so it could help other newborns. They turned to David Hoganson, MD, a cardiac surgeon who oversees a team that uses engineering and 3D modeling to enhance treatment approaches and techniques. The team simulated the intricate workings of various cardiovascular systems to see how the device could be tailored for different patient anatomies.
For instance, because no clinician knows exactly the amount of friction generated by the contraction of a newborn’s pulmonary wall after each heartbeat, the team instead conducted mechanical tests on the device to determine, as much as possible, the frictional forces it will face within different types of pulmonary arteries. Their calculations allow cardiologists to properly size the device for each patient so it will stay in place on a moving pulmonary wall.
Their testing also revealed the true increase of blood flow as a newborn’s pulmonary artery outgrows the device. This calculation lets cardiologists determine if they’ll need to replace a device with a larger one to continue blocking most of a newborn’s blood flow.
“The device wasn’t designed for this purpose,” Hoganson says. “We’ve found a way to make it work.”
Building a bridge for those who didn’t have one
Maschietto and Baird have implanted the PA flow restrictor in 17 newborns altogether, most of whom faced high risks if they had surgery after birth. Thirteen were eventually “bridged” to surgery and one is awaiting surgery. The devices can be easily removed by catheterization or during surgery, Maschietto says.
When you’re creating a game-changer, not everyone is on board.
Other institutions have used reconfigured versions of the manufacturer’s vascular plug a few times for patients with CHD and overcirculation, but Boston Children’s is believed to be among the first to implant it in newborns who had no other treatment options, Baird says. “When you’re creating a game-changer, not everyone is on board. There will be some naysayers,” he says of industry doubts of being able to help weakened newborns with complex CHD. “But Nicola and the team persisted and persevered.”
Maschietto is thrilled that he, Baird, and their colleagues have come this far. “There are still some patients you can’t treat, but we want to make that percentage as small as possible. We want patients who historically don’t do well to have options.”
Learn more or refer a patient to the Neonatal Cardiac Surgery Program.
Related Posts :
-

A heart valve that grows along with a child could reduce invasive surgeries
Clinical trials have started for the first prosthetic pulmonary valve replacement that is specifically designed for pediatric patients and can ...
-

A 'super' new heart surgery for a super kid
When you’re the first person in the world to undergo a new type of heart surgery, you don’t ...
-

Reconstructing a chest wall, one virtual step at a time
It takes a village of clinicians and engineers to reconstruct a chest wall. It also takes a lot of 3D ...
-

Experience and innovation create a safer type of heart surgery
The Eureka moment came the day before heart surgery. Easton Schlein wasn’t an ideal candidate for a full-scale surgical ...