Going out of the box to tackle pancreatic cancer
Pancreatic cancers are deadly and hard to treat, in part because they are so often detected at an advanced stage; overall five-year survival rates are about 11 percent. Two separate labs at Boston Children’s Hospital took out-of-the-box approaches to this difficult cancer, and both uncovered some very promising leads.
Wiping out pancreatic tumors’ immune defense
Randolph Watnick, PhD, an investigator in the Vascular Biology Program, started with the insight that immunotherapy, an emerging approach for a variety of cancers, has largely failed in pancreatic cancer because the tumor microenvironment — a protective “cocoon” surrounding the tumor — secretes multiple factors that block immune responses.
Watnick’s team previously showed that a naturally occurring protein, thrombospondin-1 (Tsp-1), strongly inhibits growth of various tumors. They also showed that a compound called prosaposin, and compounds derived from it, can stimulate Tsp-1 to block tumor growth. (Watnick has licensed these to Vigeo Therapeutics.) But pancreatic tumors are smart: They secrete a molecule called PRSS2 that suppresses Tsp-1.

Without Tsp-1, the tumor microenvironment throws up a slew of defenses that prevent the immune system from curbing the cancer. “These cells secrete so many agents that kill or inhibit activation of immune cells that it’s hard to target all of them,” Watnick says. “The tumor can grow without fear of the immune system.”
But when Watnick’s team blocked PRSS2 in human cancer cell lines and in mice, they restored Tsp-1 expression, disabling many of the tumor’s defenses in one stroke. This enabled the immune system to suppress tumor growth.
Even more exciting, PRSS2 circulates in the blood, making it an ideal candidate to target with antibodies. And because it doesn’t normally mutate (it is merely over-expressed by tumor cells), the cancer is less likely to develop resistance to the treatment. This approach, described in Nature Communications, might also work for ovarian and triple-negative breast cancer, which have similar self-protection strategies, says Watnick.
“If we can make an antibody against PRSS2, it could potentially be a new lifeline for patients,” he says. His lab is now working to develop an antibody and is considering strategies that would combine it with prosaposin and/or immunotherapies like PD1 inhibitors.
Starving pancreatic tumors
Nada Kalaany, PhD, an investigator in the Division of Endocrinology, took a completely different tack, asking the question, “What do pancreatic tumors need to grow?” She focused on pancreatic ductal adenocarcinoma, an aggressive cancer that relies on unusual metabolic pathways to obtain nutrients.
To support their growth, pancreatic tumors must make large amounts of compounds called polyamines. Kalaany’s team showed that the tumor microenvironment lacks a key ingredient, arginine, forcing the tumors to resort to another metabolic pathway. That pathway, predominantly used in infancy and in the fasting adult intestine, requires an enzyme known as ornithine aminotransferase or OAT.
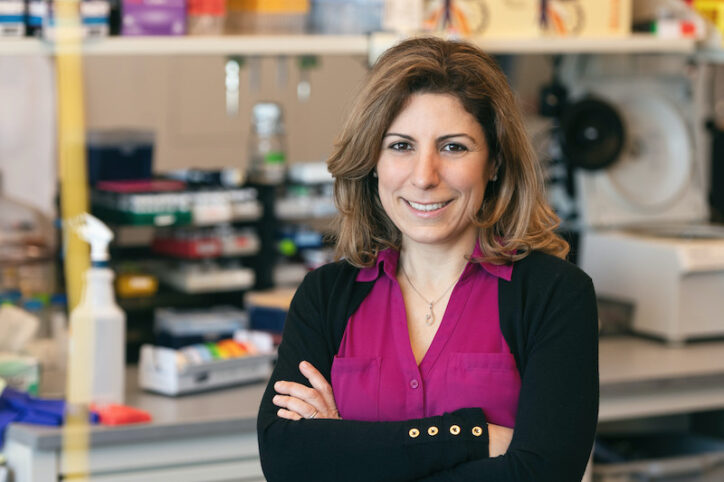
“The cancer overcomes a challenging, arginine-depleted microenvironment by using OAT to make polyamines,” explains Kalaany, who is also an associate member of the Broad Institute. “If we target OAT, we can suppress tumor growth.”
Indeed, when Kalaany’s team inhibited OAT with a drug called 5-FMO, they curbed cancer growth both in a dish and in mouse models.
The findings, reported in Nature last month, add another potential option for pancreatic cancer treatment. Targeting OAT avoids toxicity, since normal pancreatic cells don’t need OAT to make polyamines. Since 5-FMO has been used experimentally for other purposes, Kalaany sees strong potential to translate the findings to the clinic.
“Cancers always figure out a way of getting around things,” says Kalaany. “But if we target this pathway, they may not have a way to go around it.”
Learn more about research in the Kalaany and Watnick labs.
Related Posts :
-

Precision chemo-immunotherapy for pancreatic cancer?
Pancreatic cancer is highly lethal and in great need of better treatments. Only about 10 percent of patients remain alive five ...
-

'Nanobodies' from alpacas could help bring CAR T-cell therapy to solid tumors
In 1989, two undergraduate students at the Free University of Brussels were asked to test frozen blood serum from camels, and ...
-

Obesity is increasing people's risk of cancer. Why?
Obesity is now a global epidemic, and it is increasing people’s risk for cancer. The National Cancer Institute lists ...
-

Making ready-made CAR T cells for cancer immunotherapy
In CAR T-cell immunotherapy, T cells from a patient’s own blood are engineered to carry so-called chimeric antigen receptors (...





