Messenger RNA: A game-changing advance in regenerative medicine
A new way to reprogram ordinary human cells into stem cells, using RNAs, appears safer and much more efficient than current methods — and can much more readily transform stem cells into specialized cells to treat disease.
We now know that scientists can take one of your cells, perhaps a skin cell, and transform it into a cell that’s much like an embryonic stem cell – known as an induced pluripotent stem (iPS) cell. The idea is that this iPS cell could be used to make any kind of cell or tissue needed to treat your disease, that would be compatible with your immune system.
So what’s been the holdup? For starters, the current method for making iPS cells — using viruses to deliver the genes that “reprogram” your cell into a stem cell – is not only highly inefficient, but poses a risk for cancer. And the next step – turning iPS cells into different kinds of cells you might need – has proven even harder.
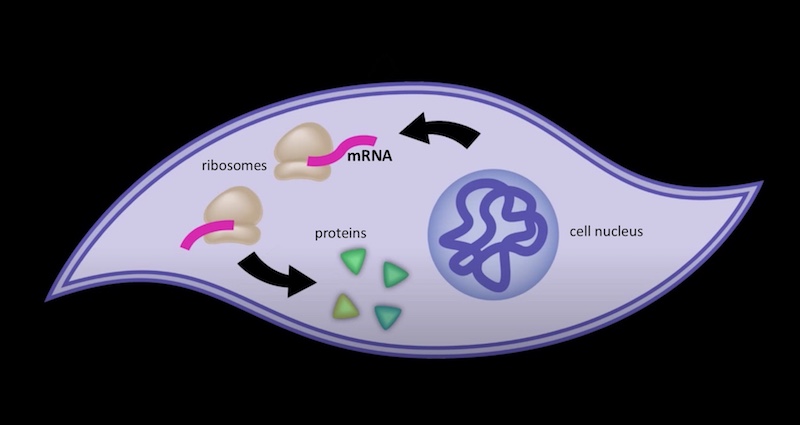
Introducing mRNA into cells
In today’s online edition of Cell Stem Cell, the lab of Derrick Rossi, PhD, of the Program in Cellular and Molecular Medicine and Immune Disease Institute at Children’s, reports a new method that might well overcome all these obstacles. Instead of genes, it puts messenger RNAs in the cells that directly instruct them to make the reprogramming proteins. These RNAs don’t hang around forever, like inserted genes do, and don’t become part of the cell’s genome, so the risk of cancer should be much reduced. And they’re up to 100 percent more efficient in reprogramming cells.
In 2006, Andrew Fire and Craig Mello shared a Nobel for the discovery of RNA interference (RNAi). This new technology is the flip side of RNAi: Whereas RNAi can block the production of abnormal or unwanted proteins, the Rossi lab’s modified RNA technique can add proteins that we want to have.
That includes not only proteins that endow that marvelous quality of “stemness,” but also factors that can drive a stem cell into different lineages or cell types – which, in the end, is what’s needed to treat people. The technology might also allow for the introduction of proteins to correct genetic diseases — without the need to use stem cells at all.
The major hurdle Rossi and colleagues had to overcome was disguising the RNAs so that cells wouldn’t perceive them as viruses and destroy them, killing the cells themselves in the process. The team spent more than a year developing synthetic, chemically modified RNAs, and showed that they successfully dodge cellular attack.
Related Posts :
-

‘Empowered to be there for Teagan’: New parents learn about hearing loss
Teagan O’Brien is a bright, spunky 4-year-old who loves reading, dancing, and playing outdoors. Her parents, Kim and Donnie, ...
-

Building better antibodies, curbing autoimmunity: New insights on B cells
When we’re vaccinated or exposed to an infection, our B cells spring into action, churning out antibodies that are ...
-

A journey through the intestine during colitis, cell by cell
Inflammatory bowel disease (IBD), causing devastating abdominal pain, persistent diarrhea, and rectal bleeding, is hard to control with current treatments. ...
-

Genetic variants are found in two types of strabismus, sparking hope for future treatment
Determining how genetics contribute to common forms of strabismus has been a challenge for researchers. Small discoveries are ...




