Trial tests dornase alfa, a cystic fibrosis drug, for severe COVID pneumonia
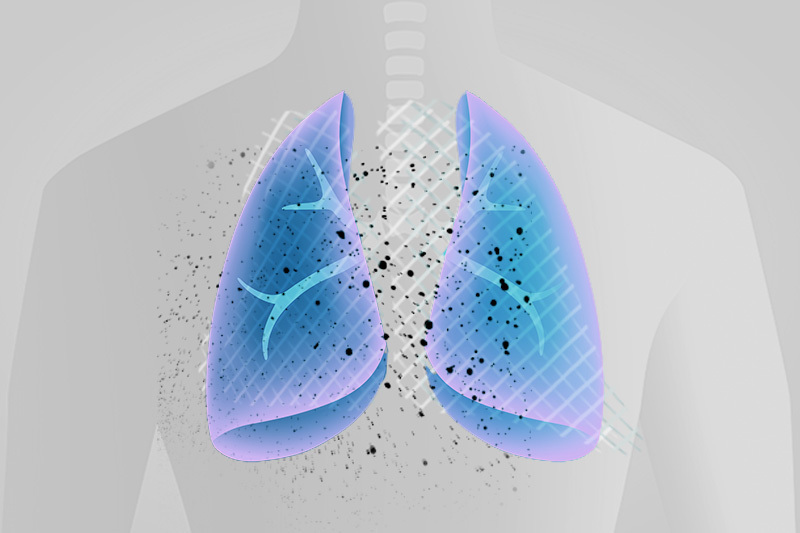
Boston Children’s Hospital and Brigham and Women’s Hospital will soon begin testing an existing drug, dornase alfa, in patients with severe COVID-19 pneumonia and respiratory failure. The randomized, controlled clinical trial aims to enroll 60 adults and children over age 3 who require mechanical ventilation.
· A randomized trial is testing whether a cystic fibrosis drug can help people with severe COVID-19 pneumonia.
· The drug breaks up thick mucus, and may break up neutrophil extracellular traps (NETs), which can cause blood clots and may increase lung inflammation
Dornase alfa (DNase 1 or Pulmozyme) is FDA-approved for cystic fibrosis to break up thick mucus secretions and prevent lung infections. The drug may also break up neutrophil extracellular traps or NETs, which scientists believe contribute to lung inflammation. (More on that below.)
“We hope this drug, which is known to be safe, will help reduce the inflammation that contributes to worsening respiratory distress in COVID-19,” says lead investigator Benjamin Raby, MD, MPH. Raby is chief of pulmonary medicine at Boston Children’s.
Hoping to get patients off the ventilator
The 18-month study will randomize patients to dornase alfa or placebo (a saline solution) soon after placement on a ventilator. Patients will receive twice-daily nebulized treatments, given through the ventilator tubing. Raby and colleagues will monitor them for up to 28 days, or until they come off the ventilator, whichever is sooner. Neither the researchers nor the patients (or their families) will know which treatment is being given.
The main outcome being tracked is how many patients in each group are alive and ventilator-free at 28 days. Other measures include airway resistance to breathing, lung compliance (the lungs’ ability to stretch and expand), blood oxygenation, and length of stay in the ICU and hospital.
Dornase alfa, NETs, and COVID-19 pneumonia
Dornase alfa is known to soften thick mucus, which some patients with COVID-19 pneumonia produce in large amounts. It therefore might make it easier to deliver oxygen through the ventilator. But the drug may have an additional benefit: breaking up NETs.
NETs are webs of DNA and toxic protein that neutrophils, first-responder cells in the immune system, spew out to entrap microbes. But NETs have a down side. They can produce dangerous blood clots in the lung, such as those that form in COVID-19 patients. These clots can contribute to lung inflammation and lung injury.
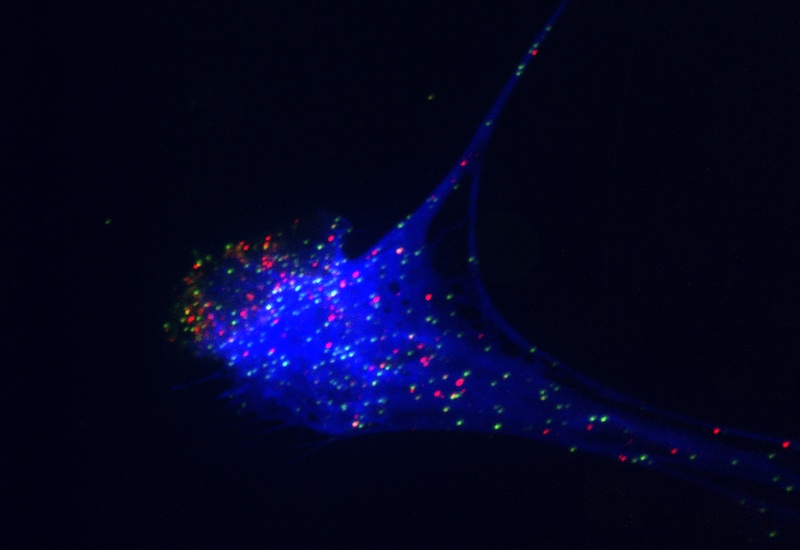
Denisa Wagner, PhD, of the Program in Cellular and Molecular Medicine at Boston Children’s, helped initiate the new trial. Her lab has been studying NETs for more than a decade, and has implicated NETs in unwanted clot formation and fibrosis (thickening and scarring of tissue). Wagner’s findings, and those of others, suggest that DNase 1 could benefit COVID-19 patients with severe lung injury.
“Preclinical studies have found that DNase 1 improved outcome in lung injury models and in thrombotic (clotting) models,” Wagner says. “These models mimic events that occur frequently in COVID-19, such as deep vein thrombosis, stroke, and microvascular thrombosis.”

While the new study focuses on the lung, scientists hypothesize that NETs contribute to excess clotting seen elsewhere in the body in COVID-19.
Genentech is providing the drug as well as supplementary financial support. The Massachusetts Consortium on Pathogen Readiness is also supporting the trial. Other study principals include Rebecca Baron, MD, and Laura Fredenburgh, MD, of Brigham and Women’s, and Meera Subramaniam, MD, and Gregory Sawicki, MD, of Boston Children’s.
Read more about the clinical trial and COVID-19 research at Boston Children’s.
Related Posts :
-

Three ways to ensure your child has the proper asthma medication
Children who have asthma should always have access to medication. But a manufacturer’s decision to stop producing a popular ...
-

BRD7 research points to alternative insulin signaling pathway
Bromodomain-containing protein 7 (BRD7) was initially identified as a tumor suppressor, but further research has shown it has a broader role ...
-

When diagnosis is just the first step: The Brain Gene Registry
Through advances in genetic sequencing, many children with rare, unidentified neurodevelopmental disorders are finally having their mysteries solved. But are ...
-

Ductus arteriosus stenting could help severely ill infants with pulmonary arterial hypertension
Treatment for infants who have severe pulmonary arterial hypertension (PAH) is sometimes limited. Because they haven’t physically ...