Exposing a tumor’s antigens to enhance immunotherapy
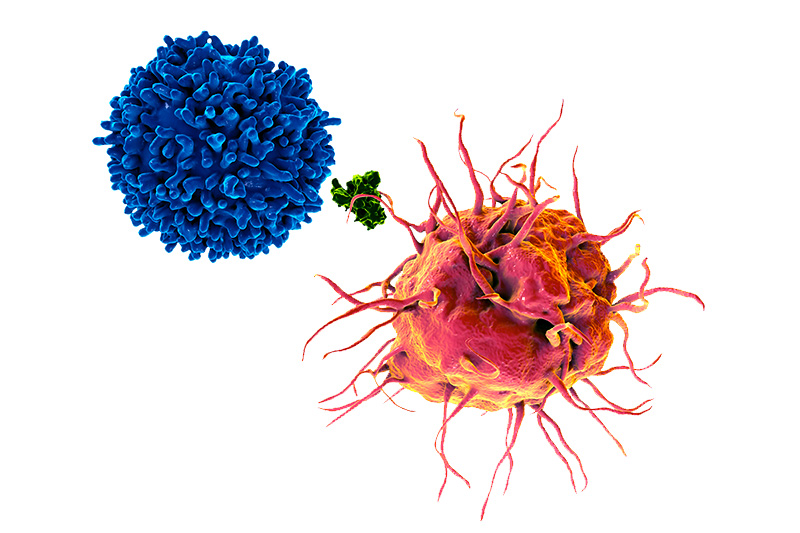
Successful immunotherapy for cancer involves activating a person’s own T cells to attack the tumor. But some tumors have a trick: They hide themselves from the immune system by preventing their antigens from being displayed, a necessary step in activating T cells. In new work published in Science, researchers in the Program in Cellular and Molecular Medicine at Boston Children’s Hospital found a way around this defense.
Led by Florian Winau, MD, the team first showed that a protein called prosaposin is critical in enabling dendritic cells to present tumor antigens to the immune system.
“Tumor tissue contains a large percentage of dying cells that shed vesicles containing tumor-derived antigens,” Winau explains. “These vesicles are taken up by dendritic cells. We found that saposins, molecules derived from prosaposin, are needed to digest these vesicles and free the tumor antigen for display to the immune system.”
Getting tumor antigens out of hiding
Through further experiments, the researchers found that tumors hide their antigens by loading prosaposin with chains of sugar molecules, causing prosaposin to be secreted from dendritic cells. This has the effect of depleting saposins, preventing the vesicles from being digested and tumor antigens from being released. And that enables tumors to evade immune detection.
The team’s logical next step was to try adding prosaposin back. In a mouse melanoma model, giving prosaposin intravenously, coupled to an antibody that targets dendritic cells, enabled the animals’ immune systems to once again detect the tumor antigens and activate T cells. When the researchers combined prosaposin with immune checkpoint inhibitor drugs, they saw reduced tumor growth.
Winau and colleagues have filed for a patent on the technology. Working with an industry partner, they have devised a targeted system to deliver prosaposin and hope to develop a candidate drug to test in clinical trials.
In a separate project, they’re working on a diagnostic test that would detect sugar-coated prosaposin in the blood. This would indicate that antigen presentation is impaired and that the tumor is escaping immune attack, meriting a change of treatment.
Pankaj Sharma, PhD, Xiaolong Zhang, PhD, and Kevin Ly of PCMM were co-first authors on the paper. For inquiries on the technology, contact Michael Bergin, PhD, MBA, in the Technology and Innovation Development Office.
Explore projects in the Winau Lab and more research at PCMM.
Related Posts :
-

Combining CAR-T cells and inhibitor drugs for high-risk neuroblastoma
Chimeric antigen receptor (CAR)-T cell therapy is a potent emerging weapon against cancer, altering patients’ T cells so they ...
-

Making immunotherapy safe for AML
Acute myeloid leukemia (AML), the second most common leukemia in children, is hard to treat and has a five-year survival ...
-

Making ready-made CAR T cells for cancer immunotherapy
In CAR T-cell immunotherapy, T cells from a patient’s own blood are engineered to carry so-called chimeric antigen receptors (...
-

Going out of the box to tackle pancreatic cancer
Pancreatic cancers are deadly and hard to treat, in part because they are so often detected at an advanced stage; ...