An off-the-shelf tamponade kit provides surgeons with ‘the luxury of time’ during a life-threatening emergency

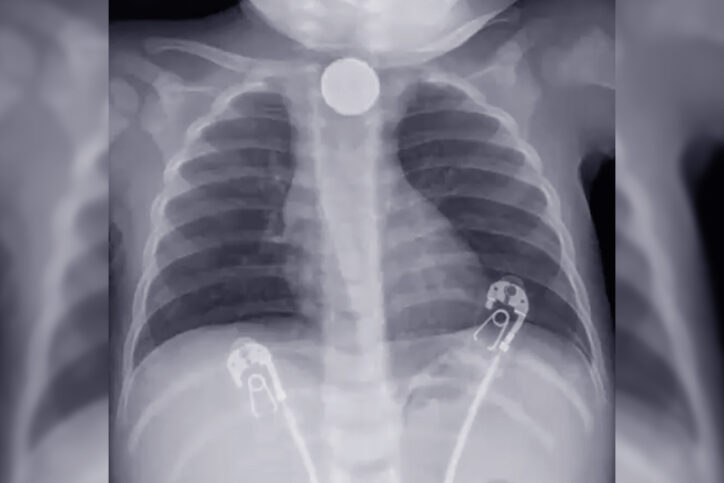
It was a late Friday afternoon in April when the call came: A young boy was being transferred to Boston Children’s emergency department after swallowing a button battery. Although his mother had previously taken him to another local hospital when she noticed he wasn’t eating or drinking much, the battery ingestion had been missed until an x-ray there earlier that day. By the time the child, a 13-month-old named Nathan, arrived at Boston Children’s, he was in critical condition — vomiting blood and having seizures.
The trauma team in the ED — including general surgeons, cardiac surgeons, nurses, gastroenterologists, and otolaryngologists — knew that time was of the essence: With Nathan near death, they needed to stop the bleeding and get him to the operating room as soon as possible.
The devastating potential of button batteries
Benjamin Zendejas-Mummert, MD, MSc, was about to head home after a long day when he caught wind of Nathan’s case. “I was just a nosy bystander,” says Zendejas-Mummert, who is surgical director for the hospital’s Esophageal and Airway Treatment (EAT) Center. “I wandered over to the ED to see what was going on and if I could help.”
Zendejas-Mummert’s colleague Peter Ngo, MD, the EAT Center’s medical director, was working that weekend and also sprang into action. The two physicians are all too familiar with the devastating potential of button battery ingestion: When consumed, these batteries can become lodged in the body. Their electrical current creates an alkaline environment, which can burn through the soft tissue of the esophagus and aorta, often resulting in permanent difficulty eating and drinking, infection, and death. In many cases, ingestion can lead to large hemorrhages that can be fatal — even when they occur in medical settings.
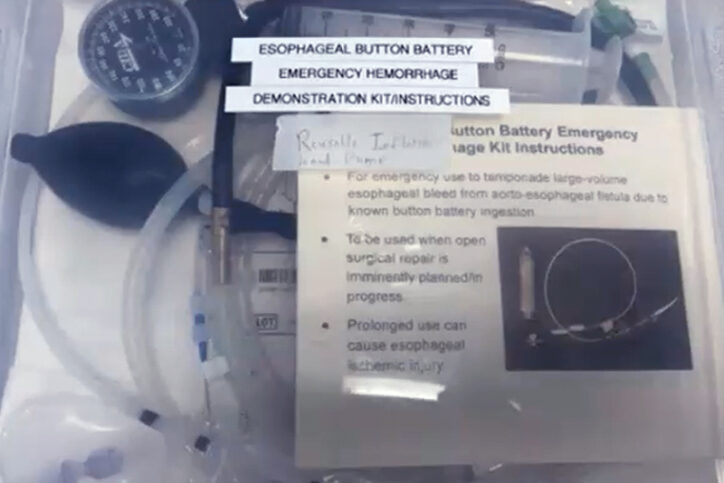
A child-sized kit that stems bleeding
Within 20 minutes, Nathan was transported from the ED to the OR for surgery. In the OR, Zendejas-Mummert and Ngo turned to a kit they had recently designed just for such scenarios. The concept of the kit, which contains a balloon tamponade aimed at stemming esophageal bleeding, isn’t new: Similar devices are widely used in adults. But based on an earlier case in which a young child died after swallowing a battery, the pair created a kit specifically sized for children. Now they would put it to the test.
With the kit at the ready, the team successfully removed the battery from where it was lodged in Nathan’s esophagus. But there was another concern: Two large blood clots had formed in the area and needed to be removed. As expected, their removal resulted in a massive hemorrhage — and that’s where the tamponade came in.
“After guiding the device down the esophagus, we inflated the balloon, which immediately stopped the bleeding,” explains Ngo. “The balloon remained inflated for the entire duration of the surgical intervention.” That gave the team the luxury of time to operate and thoroughly address Nathan’s injury.
A case where stars aligned
Because the source of the bleeding was initially unclear, cardiac surgeon Michael Kwon, MD, also scrubbed in to open the chest and ensure optimal control of the bleeding vessel. “We had the cardiac OR team at the bedside in case we needed to perform heart-lung bypass,” he says.
Because Ngo was able to control bleeding with the balloon, Kwon and Zendejas-Mummert had time to safely identify the source of bleeding and transition to conventional surgical control of the bleeding through chest and neck exposure without requiring bypass. With this achieved, they were able to dissect the esophageal fistula that had formed, debride the left carotid artery, place a bovine pericardial patch on the carotid, and repair the esophagus.
Following surgery, Nathan remained in the hospital for 28 days and underwent seven esophageal endoscopic dilations. The effects have been dramatic: “He’s now eating everything by mouth without even a g-tube and has had no neurologic complications,” says Zendejas-Mummert. “Overall, it’s an excellent outcome.”
Nathan’s mother is more candid: “I believe I would have lost my son at any other hospital,” she says.
It’s a result that Zendejas-Mummert attributes to Boston Children’s multidisciplinary team approach. “Despite it being a Friday afternoon, with everyone getting ready to go home, we had an abundance of resources, expertise, innovation, and communication,” he says. “This was a case where all the stars really aligned.”
Learn more about the Esophageal and Airway Treatment Center.
Related Posts :
-

Tiny, shiny, and dangerous: What families should know about button batteries
Button batteries may be bright, shiny, and eye catching, but they also have a dark side — especially for kids. Look ...
-

Beyond limits: A staged approach to jejunal interposition
By the time Chase Essex arrived at Boston Children’s Hospital in 2016, he had reached what most clinicians would consider ...
-

Game-changing surgical procedure results in zero-percent TEF re-recurrence rate
A tracheaesophageal fistula (TEF) is a congenital defect in which an abnormal connection forms between a child’s esophagus and ...
-

Predicting feeding difficulties in children with esophageal atresia: A proactive approach
Children with esophageal atresia are at risk for developing anastomotic strictures, or areas of esophageal narrowing, following surgical repair. Clinicians ...





