Optimizing care for bronchopulmonary dysplasia, infant by infant

Preterm newborns with bronchopulmonary dysplasia (BPD) can require ongoing mechanical ventilation to support their lungs. But babies with BPD aren’t just newborns with underdeveloped lungs. Each has a unique presentation. And every part of their care is important, with the ultimate goal of enabling them to grow, develop, and go home to their families.
The Division of Newborn Medicine at Boston Children’s Hospital is finding success with a customized, long-term, whole-baby approach, honed through outcomes data, quality improvement initiatives, and the recognition that each infant’s lung disease has unique characteristics.
“Our strategy is pro-growth,” says Kristen Leeman, MD, associate medical director of Boston Children’s NICU. “Our goal is to optimize care with a focus not only on the lungs, but also the baby’s growth and neurodevelopment.”
Nutrition is a key component of care, supporting growth of both the lungs and the baby. An individualized approach to respiratory support is also important as lung physiology can change.
“We want to prevent ventilator injury to the lung,” says Jonathan Levin, MD, who has appointments in both Newborn Medicine and Pulmonary Medicine. “But at some point during development, we may need to shift the strategy to adequately supporting the baby.”
Another QI effort involves optimizing the timing of tracheostomy. “Delaying tracheostomy can increase length of stay and impair neurodevelopment,” says Leeman. “We’re trying to recognize earlier when infants need long-term respiratory support so we can get them home sooner.”
Xavien: A case study
Xavien Velazquez’s case is illustrative. Born at 26 weeks gestation, he came to Boston Children’s NICU in October 2021, two months after he was born. He had been having two to three daily “coding” events at his birth hospital in which he stopped breathing.
“Xavien had very underdeveloped lungs and needed breathing support, but there were elements of his BPD that weren’t typical,” says Levin. “He had apnea, desaturation, and bradycardic episodes where his heart rate would very quickly drop. He would have to be re-intubated and get chest compressions. His team was suspicious that something was wrong with his airway.”
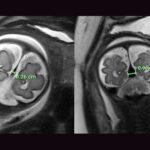
Arriving at Boston Children’s at 33 weeks post-menstrual age, Xavien had a dynamic bronchoscopy to look into his airway as he breathed and see the impact of real-time adjustments in ventilator pressure. The bronchoscopy was done with Xavien actively breathing. “We wanted to mimic real life as much as possible,” says Levin.
The bronchoscopy showed that Xavien’s BPD was complicated by tracheomalacia, or near-complete collapse of his airway during exhalation, mostly in the tracheal area.
“Malacia can be a complication of chronic ventilation support,” says Levin. “A weakening of cartilage in the airways may also go along with underdevelopment of the lungs or be caused in part by steroids. Once we identified malacia, we were able to titrate Xavien’s ventilator settings to stop him from having these life-threatening episodes. We also recognized that he was a candidate to have his tracheomalacia surgically repaired.”
Rethinking ventilation
Many NICUs are uncomfortable using high pressures when they ventilate newborns. But the team felt that a high positive-end expiratory pressure (PEEP) would allow Xavien to grow and thrive until he was big enough to have surgery. The team therefore increased his PEEP to 18 cm H2O.
“He had only been on PEEP 8 before, so every time he got upset his airways would collapse like a pancake and he couldn’t breathe,” Levin says. “We figured out a ventilator setting that allowed him to grow, participate in physical therapy, and interact more with his family.”
With more ventilatory support, Xavien also needed less sedation.
“While sedation helped keep him from panicking and hyperventilating, we felt too much might interfere with his development,” says Levin. “He had a relatively smooth time in the NICU once he was on the right settings.”
Maximizing Xavien’s development
On November 12, about a month after Xavien’s arrival, his team moved ahead with a tracheostomy to provide more secure ventilatory support and keep Xavien stable until he was big enough for surgery. Equally important, it freed up his mouth and face, allowing him to develop oral-motor skills and, again, interact more with his parents.
Recognizing early that Xavien would benefit from a tracheostomy allowed him a stable period of time in which he made important developmental strides. His ventilator settings were too high to safely leave the hospital, but a surgery to open his airways might allow him to do so.
In January 2022, four months after birth and just past his due date, Xavien was ready for surgery: a tracheopexy to open his collapsing airway, performed by Benjamin Zendejas-Mummert, MD, of the Esophageal and Airway Treatment Program. The operation sutured the back portion of Xavien’s trachea to his spine to provide structural support.
After recovery from his surgery, Xavien was able to have his ventilator settings lowered into a range where he could be cared for safely at home by his family.
Discharging Xavien
Normally, Xavien would have been sent to a rehabilitation hospital to recover from the tracheopexy. But the nursing team, led by Theresa Andrews, RN, felt that with the improvement Xavien made after surgery, he could skip the months of rehab and go directly home. Being home would help him thrive developmentally.
Xavien’s parents were already participating actively in his care, visiting daily and handling much of his tracheostomy and G-tube care. Before Xavien’s discharge, they underwent further intensive preparation under the guidance of Christina Cavanaugh, RRT, in the Chronic Ventilation and Neuromuscular Program.
Each parent had a 24-hour “dress rehearsal” in the NICU, where they were responsible for all of Xavien’s care (with staff available as a backup). Through simulations in the SIMPeds lab, they practiced handling emergency scenarios while NICU case manager Karen Cote, RN, coordinated home equipment and services for the family through multiple agencies.
Xavien was discharged in March 2022, closely followed through a mix of telehealth and in-person visits by Levin, Cavanaugh, and Kathryn Malpocher, PNP, in the Chronic Ventilation and Neuromuscular Program. He is still on the ventilator 24/7, but on lighter settings. The plan is to wean him off and eventually remove the tracheostomy tube.
The attention to Xavien’s development has paid off. Though he does have some delays, he has scored high on social/emotional measures.
“None of us have a crystal ball,” says Levin, “but he’s as best set up for success as he can be.”
Explore the Division of Newborn Medicine at Boston Children’s.
Related Posts :
-

“Observe. Be open.”: How Boston Children’s nurses are changing the future of global health
Ashley Birch, MSN, CPNP, a Boston Children’s pediatric nurse practitioner and Global Nursing fellow, didn’t expect a trash ...
-

Could the falcine sinus hold the key to vein of Galen outcomes?
A Boston Children’s Hospital study uncovers how fetal magnetic resonance imaging (MRI) could be a game-changer in predicting outcomes ...
-

Using her voice: After tracheomalacia treatment, Claire keeps her eye on the ball
Claire Kantany is only 10, but she knows what she wants to do when she grows up — in fact, she’...
-

Modifying macrophages in the lung could head off pulmonary hypertension
In the 1980s, when Stella Kourembanas, MD, began her career in neonatology, she cared for newborns with pulmonary hypertension, a ...