Tackling an aggressive, treatment-resistant lymphoma where it lives
Anaplastic large cell lymphoma, a form of non-Hodgkin lymphoma, is the most common aggressive lymphoma in children. Chemotherapy and radiation fail to cure about 30 percent of cases. When tumors are driven by the oncogene ALK — which is the case for the majority of children — kinase inhibitor drugs like crizotinib are very effective in blocking tumor growth. They also lack the serious side effects of chemotherapy.
However, ALK inhibitors also very expensive – about $80,000 a year – and must be taken for a lifetime. As soon as they’re stopped, the lymphoma comes back. Roberto Chiarle, MD, a hematopathologist and researcher at Boston Children’s Hospital, wanted to know why.
“ALK inhibitors can control the lymphoma, but you cannot reach a cure,” he says. “Why do lymphoma cells persist for so long?”
The answer he found, reported in Science Translational Medicine, has sparked plans to test a new combination therapy in patients with relapsed anaplastic large cell lymphoma. Down the road, Chiarle hopes, it might even avoid the need for chemotherapy.
Probing a lymphoma’s safe haven
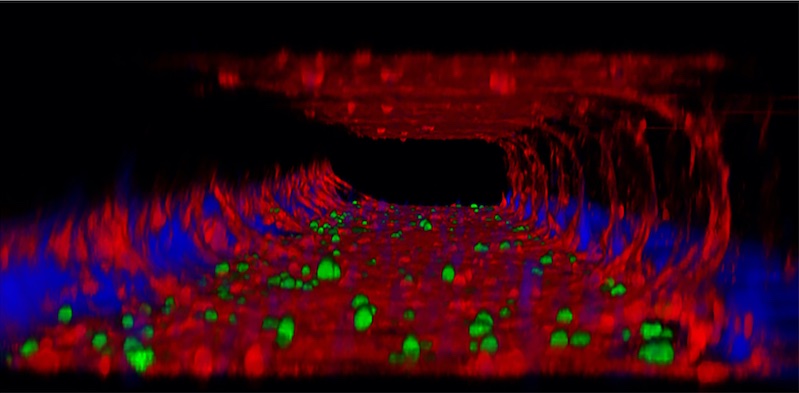
Chiarle and his collaborators at the University of Torino in Italy knew that persisting lymphoma cells tend to hang out around blood and lymphatic vessels.
“When they sit in the proximity of the vessels, they are protected,” says Chiarle. “We thought, maybe the microenvironment around the vessels is protecting these cells.”
Thus began a series of experiments. For some, the researchers created a three-dimensional microfluidic model of a vessel on a chip, lined with endothelial cells. They added lymphoma cells and showed that when they were lodged in the vessel, ALK inhibitors didn’t kill them.
They further found that endothelial cells produce two proteins, CCL19 and CCL21, that enable lymphoma cells to survive, even as kinase inhibitors keep the cells from growing and spreading. The survival signal is weak: Only cells close to the vessels receive enough of it. But is enough to keep the cells alive. When the proteins were taken away in lab experiments, the cells underwent apoptosis and died.
“ALK inhibitors are very potent against lymphoma,” says Chiarle. “But when you suspend them, the cells immediately start to duplicate and proliferate again.”
The team showed that the CCL19 and CCL21 signals activate PI3K via the CCR7 receptor. Blocking this pathway — either by deleting the gene for the receptor or by inhibiting PI3K — killed the persisting lymphoma cells.
Serendipitously, one PI3K inhibitor, the drug duvelisib, is currently used clinically in leukemia and other forms of lymphoma. When Chiarle and colleagues combined duvelisib with crizotinib and gave the drugs to mice with human anaplastic large cell lymphoma, many animals were cured.
“Others eventually developed lymphoma again, but much later in time,” says Chiarle. “By optimizing this combination, we hope to increase the percentage that will be cured.”
Clinical trial planned
A Phase 1 clinical study of crizotinib plus duvelisib is now in the planning stages for children and adults with anaplastic large cell lymphoma in whom chemotherapy has failed. It will possibly be run through the Leukemia & Lymphoma Society’s multicenter grant network, which funded the current study.
Chiarle hopes this and other work will eventually enable patients to be treated without chemotherapy, avoiding toxicity and the risk of secondary cancers.
“ALK inhibitors work beautifully as a first-line treatment in other cancers, and we think that combining them with duvelisib could provide a chemo-free cure for a good fraction of anaplastic large cell lymphomas,” he says. “That’s important especially for children who will live for decades.”
Learn more about research in the Chiarle Lab or refer a patient to Dana-Farber/Boston Children’s Cancer and Blood Disorders Center
Related Posts :
-

A potential danger of CRISPR gene editing — and why base editing may be safer
Gene therapy using CRISPR/Cas9 gene editing is currently in clinical trials around the world for a variety of diseases, ...
-

Going out of the box to tackle pancreatic cancer
Pancreatic cancers are deadly and hard to treat, in part because they are so often detected at an advanced stage; ...
-

An unexpected journey reveals a potent way to attack tumors
Research on the effects of prenatal exposure to the Zika virus has yielded an unexpected dividend: a potentially promising way ...
-

A new cancer mechanism: Failed cellular housekeeping
Cancer can stem from mutations in many different genes. New research from Boston Children’s Hospital and Dana-Farber Cancer Institute ...