Specialized T cells protect against the deadliest form of malaria
Each year, there are about 230 million cases of malaria globally. Children under the age of 5 are at highest risk of serious illness and death, accounting for about 265,000 deaths, or nearly 70 percent of all malaria deaths worldwide. Despite significant time and money poured into efforts to develop an effective malaria vaccine, the world still waits.
In new research, Caroline Junqueira, PhD, — a visiting scientist from Brazil — and other scientists in the laboratory of Judy Lieberman, MD, PhD, of the Program in Cellular and Molecular Medicine (PCMM) discovered that a type of lymphocyte in the blood appears to protect against blood-stage malaria. During this critical phase of the disease, symptoms develop and the disease spreads throughout the body. Their team discovered that this lymphocyte was able to destroy red blood cells infected by the parasite Plasmodium falciparum found in Africa. They hope to use this new information to help develop an effective malaria vaccine. This research was published in Nature Immunology.
A two-pronged approach to protection

Lymphocytes are part of the body’s immune system and they come in two general varieties: T cells and B cells. Lieberman’s lab discovered two previously unknown ways that a special type of unconventional T lymphocyte, called gamma delta T cells, protect against blood stage malaria.
“It’s sort of a double whammy,” says Lieberman. “We found that the gamma delta T cells can recognize blood cells that are infected with malaria in two ways we didn’t know before — direct killing and also by phagocytosis (or engulfing them).”
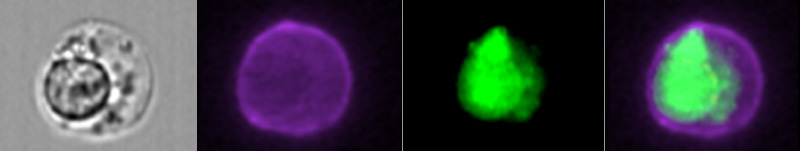
First, they recognize a metabolic product made by the malaria parasite within infected red blood cells. The gamma delta T cells can rupture these red blood cells, killing the parasites inside. Second, they also detect infected red blood cells coated with anti-malaria antibodies. Once they detect the antibody-coated blood cells, the gamma delta T cells engulf the infected cell, killing it and stopping further spread of the parasite within the body.
Higher numbers lead to vaccine protection

Researchers already knew that gamma delta T cells are found in high numbers in people already infected with malaria; in some cases, they can make up to about 30 percent of all the lymphocytes in the body. Infection activates these lymphocytes, causing them to increase in numbers and to kill infected red blood cells.
Research has already established that having higher numbers of these delta gamma T cell lymphocytes in the blood before vaccination determines whether or not malaria vaccines work in normal volunteers. “However, it was perplexing why this was so,” says Junqueira. “This new study explains how antibodies against the parasite, generated by vaccination, that coat infected cells can cause them to become targets for removal by the immune system.”
Protection against blood-stage malaria
After a bite, the parasite from an infected mosquito first settles in the liver where it replicates before releasing large parasite numbers into the blood.
“Most malaria vaccines have focused on the liver when the numbers of parasites are low and controllable,” says Lieberman. “Once it’s in the bloodstream the infection goes crazy; nobody thought that there was an immune response to the parasites in red blood cells because red blood cells lack surface proteins recognized by most conventional lymphocytes.”
However, Junqueira and Lieberman previously discovered that conventional lymphocytes called killer T cells, recognized a different strain of malaria, Plasmodium vivax, in infected blood cells. “But, killer T cells did not recognize Plasmodium falciparum-infected red blood cells,” says Junqueira. “However, gamma delta T cells did, and provided protection.”
Boosting gamma delta T cells prior to infection
From this research, the team is looking at ways to increase the number of gamma delta T cells before infection as a way to improve protection with vaccination. “One way to do this might be to choose an immune stimulant called an adjuvant that activates gamma delta T cells and add it to a malaria vaccine,” says Junqueira.
Other contributors to this research include Rafael B. Polidoro, Guilherme Castro, Sabrina Absalon, Zhitao Liang, Sumit Sen Santara, Ângela Crespo, Dhelio B. Pereira, Ricardo T. Gazzinelli, and Jeffrey D. Dvorin.
Read more about research from the PCMM.
Related Posts :
-

Building better antibodies, curbing autoimmunity: New insights on B cells
When we’re vaccinated or exposed to an infection, our B cells spring into action, churning out antibodies that are ...
-

Could SIDS be caused by unrecognized brain infections?
Some infants who pass away from sudden infant death syndrome (SIDS) are known to have had acute minor infections. Could ...
-

Exposing a tumor’s antigens to enhance immunotherapy
Successful immunotherapy for cancer involves activating a person’s own T cells to attack the tumor. But some tumors have ...
-

Could a GI bug’s toxin curb hard-to-treat breast cancer?
Clostridium difficile can cause devastating inflammatory gastrointestinal infections, with much of the damage inflicted by a toxin the bug produces. ...