First-of-its-kind pressurization test could improve Ross procedure outcomes
The Ross procedure is a preferred surgery to treat severe aortic valve disease. The procedure replaces the failing valve with a patient’s own pulmonary valve.
It’s an effective treatment option, but some patients have had complications. After surgery, the root of their aortic valve — where the valve connects with the heart — enlarges and causes blood to regurgitate, forcing the heart to work harder than it should.
Key takeaways
- Boston Children’s developed a surgical technique that pressurizes a pulmonary valve to see if it will withstand increased blood pressure as an aortic valve.
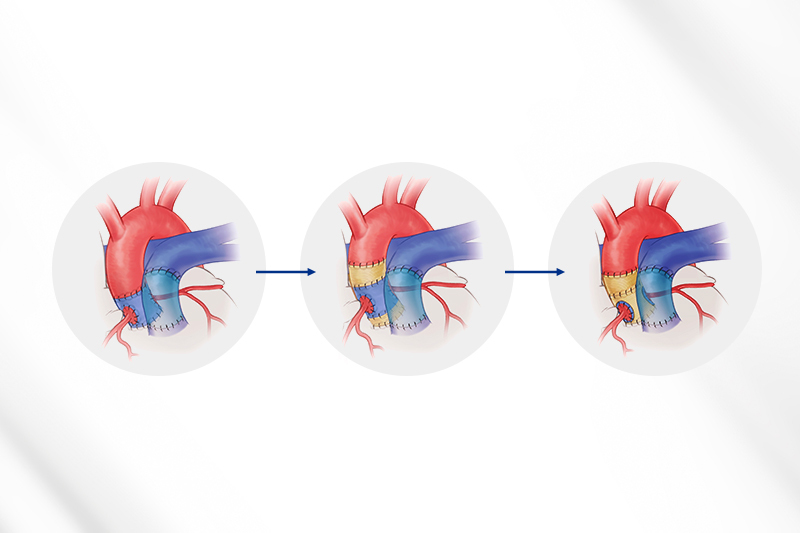
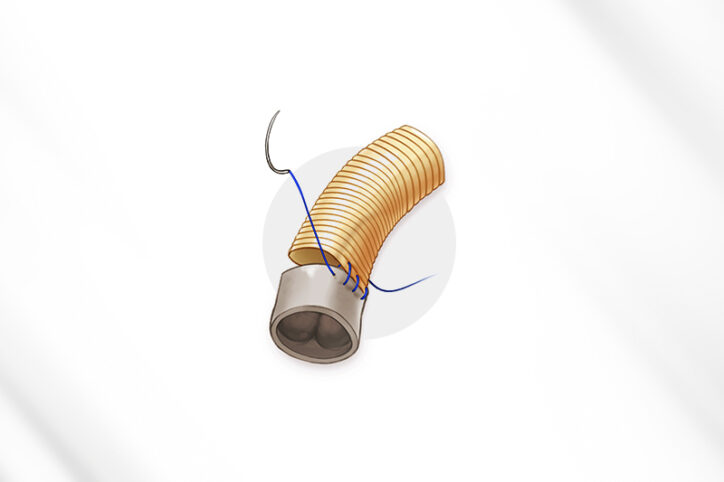
- This Ross procedure technique includes customizing prosthetic material into a reinforcing wrap to help the valve and its root stay durable, potentially preventing regurgitation.
- The technique also allows patients at greater risk of regurgitation to have the procedure.
Boston Children’s heart surgeons recognized that new approaches to the Ross procedure over the years hadn’t significantly reduced aortic root dilation, so they developed a technique that gets ahead of the problem. During surgery, they perform a pressurization test on a pulmonary valve to see if it can be converted to an aortic valve. If the test indicates a valve is strong but could experience regurgitation, the surgeons reinforce it with custom-fit prosthetic material during the procedure.
Boston Children’s is the first hospital to test and modify a pulmonary valve during a Ross procedure. Early results from a recent study of adult patients are promising: Most have had no regurgitation. “We are anticipating the unanticipated,” says cardiac surgeon Sitaram Emani, MD, who developed the technique. “Once you move a pulmonary valve into a high-pressure setting with the aorta, it may not work as well. We want to make sure it does.”
A pass-or-fail test during surgery
“Many valve failures after a Ross happen when the aortic root dilates over time, which separates the valve leaflets and creates a gap in the middle, causing leakage,” says cardiac surgeon Michael Kwon, MD. The new technique ensures a valve immediately functions well and stays durable over time, steps that he says can prevent leakage and regurgitation.
Pressurization assesses whether a patient’s pulmonary valve and its root can withstand a shift from the lower pressure pulmonary system to the higher pressure arterial system. In that high-pressure setting, the valve needs to open and shut properly about 100,000 times a day while not having any significant leakage.
The test starts with a perfusionist using an added line on a bypass machine to direct blood flow to the pulmonary valve and its root. This first round of testing evaluates the valve’s overall condition. If it’s apparent the valve won’t handle arterial pressure, it is put back into its original position. Surgeons instead replace the aortic valve with a prosthetic valve.
If a valve has potential but needs modification to handle arterial pressure, the surgeons reinforce it with prosthetic tubing and pressurize it again, this time with more force. If the valve passes this stage, they wrap it in more custom-fit prosthetic material that will stabilize the valve and its root when they are placed between the aorta and left ventricle. The valve and root then undergo one more round of pressurization. If they hold strong, the valve is implanted.
“This is the kind of innovation that changes what’s possible for patients with complex aortic valve disease,” says cardiac surgeon Christopher Baird, MD, director of Boston Children’s Congenital Heart Valve Program. “By understanding how a valve responds under real pressures before we implant it, we are preventing complications, rather than reacting to them — giving more patients the opportunity for a durable, lifelong solution.”
Making more patients eligible for aortic valve treatment
It’s not the first time the cardiac surgery team has revised the Ross procedure to reduce the chance of complications. The Ross has too much value to abandon, Kwon says.
The idea for the latest revision came to Emani as he tested donated valves as part of a basic experiment in a lab. As he looked at the bottom of a pulmonary valve while it was being pressurized, he thought, ‘Why can’t we do this during a Ross procedure?’”
Now that idea is showing promise. As Emani, Kwon, and other Boston Children’s heart specialists detail in The Journal of Thoracic and Cardiovascular Surgery, three adult patients whose Ross surgery included the pressurization-reinforcement technique didn’t experience regurgitation, while a fourth patient had minor regurgitation.
Aside from improving outcomes for patients who are ideal Ross candidates, the technique also opens a door for those who normally aren’t considered for the procedure, Emani says. That includes those who have hypertension, a large aorta, or leakage with their original aortic valve.
“Those conditions don’t affect surgery because we’re able to find a solution and support the valve in a way that doesn’t lead to dysfunction,” Emani says. “More patients can have the Ross because we can help the valve withstand those traditional risk factors.”
Learn more about the Department of Cardiac Surgery or refer a patient.
Related Posts :
-

Constant improvements make the Ross procedure a safe aortic valve replacement option
Cardiac surgeons understand that innovation isn’t always about invention. Improving something can be just as transformative. So it shouldn’...
-

Treating MAPCAs with unifocalization surgery and cardiology care
Children born with a rare form of tetralogy of Fallot (ToF) face a challenging type of congenital heart ...
-

It's all in the PV loops: New analytical model could improve circulation assessments before heart surgery
The double-switch operation corrects the congenital reversal of the heart’s ventricles and its two main arteries. It’...
-

Conduction tissue mapping is shown to significantly reduce heart block
New research by Boston Children’s validates an innovative approach to mapping the heart’s invisible conduction tissue during surgery. ...