Taking charge: Emma perseveres with laryngeal cleft

Emma Morris is “a pistol,” says her mother, Sarah. “She’s a spitfire, passionate and caring.” But the 11-year-old gets anxious, too — and for an understandable reason. She’s been in and out of the hospital since she was a newborn. In fact, Sarah estimates that her daughter has spent more than 400 nights at Boston Children’s Hospital over the years.
Emma and her twin brother, Drew, were born prematurely. While Drew continued to grow and thrive in their birth hospital’s NICU, Emma was diagnosed with tracheoesophageal fistula (EA/TEF), two related conditions that occur when the esophagus and trachea don’t form properly. Local surgeons repaired the EA/TEF, but Emma was still struggling to gain weight and turned blue when they tried to take her breathing tube out of her. “We decided it was time to get a second opinion,” says Sarah.
A waiting game
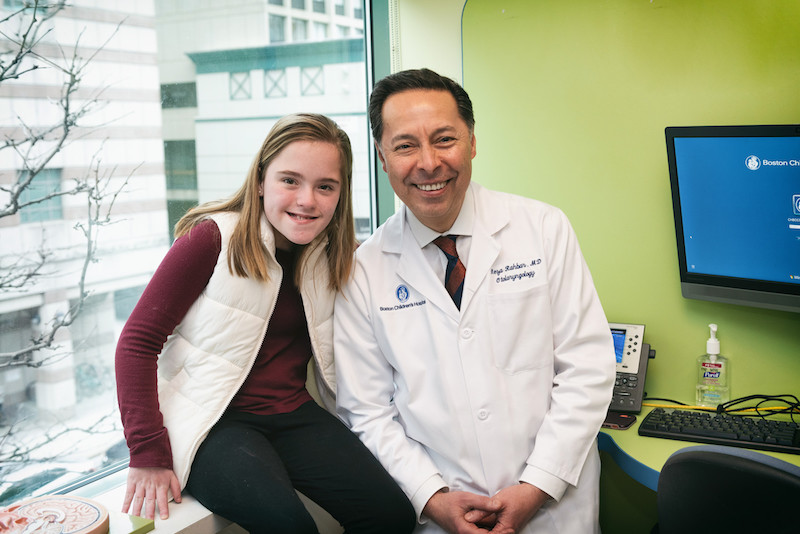
That second opinion ultimately led the family to Boston Children’s Center for Airway Disorders (CAD) and its director, Dr. Reza Rahbar, who diagnosed Emma with a type III laryngeal cleft. This abnormal opening between the larynx and the esophagus can allow food and liquid to pass through the larynx into the lungs, leading to a number of eating and breathing problems. As Dr. Rahbar explained what Sarah and her husband, Jon, could expect, “We had instant respect for him,” she says. “We knew he could help us.”
But first, the family had to wait for Emma to grow enough to undergo surgery to repair the laryngeal cleft. In the meantime, clinicians gave her a tracheostomy so she could breathe more easily. “That was really hard for us,” Sarah admits. “We didn’t want her to have to have a trach, but we knew it was what she needed until she was ready for surgery.”
After nearly 250 days, Dr. Rahbar was able to perform the repair endoscopically and, after another month of recovery, Emma could finally leave the hospital. “We were so happy to go home,” says Sarah. “But we knew we weren’t done and there would be more surgeries in her future.”

Coping with complex needs
Indeed, Emma’s cleft has continued to grow over time, requiring multiple procedures to close it. Through it all, Dr. Rahbar has been by her side, encouraging the family to be patient and have faith. “He is so invested in us, and we hold on to everything he says because it gives us hope,” says Sarah. Also on Emma’s team: Dr. Russell Jennings, nurse practitioner Leah Frain, and their colleagues in the Esophageal and Airway Treatment Center, who treat her EA/TEF and related concerns. Emma also receives monthly infusions for a primary immune deficiency.
With such complex needs, it’s natural for Emma to feel stressed and overwhelmed. She helps address the emotional aspects of her health through regular visits with psychologist Lauren Mednick in the hospital’s Medical Coping Clinic. There, she learns tools to help her relax and get through whatever is coming next and earns rewards — like a cup of hot chocolate with Mednick — for sticking with her medical regimen. “We worry as parents, but it’s totally different when you’re a kid,” says Sarah. “This clinic helps.”
In her spare time, Emma loves cooking, hanging out with friends and family, and hates missing school, where she eats lunch with her brother every day. And she doesn’t let her health hold her back. “We push her just as hard as we push Drew. We don’t give her a pass and hate it when other people do,” says Sarah. “As she gets older, she’s taking charge of her life — and that’s amazing to watch.”
Learn about the Center for Airway Disorders (CAD).
Related Posts :
-

‘The reason I became a nurse’: Maeve’s memories of laryngeal cleft repair
Being a gastroenterology nurse is more than a profession for Maeve Lee. When she cares for patients with feeding tubes, ...
-

Pushing the envelope for Eoin: Our family’s experience with esophageal atresia
When I recently brought my son, Eoin, to Boston Children’s for an appointment, we ran into Dr. Farokh Demehri ...
-

‘Sami’s trach helps him breathe’: Living with laryngeal cleft
Today, Sami is a playful toddler with so much energy that his parents need to remind him to take breaks. ...
-

Predicting feeding difficulties in children with esophageal atresia: A proactive approach
Children with esophageal atresia are at risk for developing anastomotic strictures, or areas of esophageal narrowing, following surgical repair. Clinicians ...





