‘The reason I became a nurse’: Maeve’s memories of laryngeal cleft repair

Being a gastroenterology nurse is more than a profession for Maeve Lee. When she cares for patients with feeding tubes, she’s also paying it forward. More than two decades ago, Maeve experienced many of the same challenges her patients face today.
Medical mystery
At first, Maeve seemed like a perfectly healthy newborn, but then she turned purple when her mother tried to feed her, a problem that continued every time she tried to feed. “We really did not believe it was possible she couldn’t swallow properly,” recalls her mother, Annemarie.
Swallowing problems can stem from a wide range of health issues. The challenge for Maeve’s doctors at Boston Children’s Hospital was figuring out what was causing hers. To ensure she received nutrition to help her grow, Dr. Athos Bousvaros of the Division of Gastroenterology, Hepatology, and Nutrition placed a gastronomy tube (G-tube) that delivered food directly into her stomach.

“The G-tube made our day-to-day life easier,” says Annemarie. Maeve didn’t choke when eating and didn’t fuss with the tube. This helped ease her mother and father Bill’s minds. “She just made everything seem OK, which helped us adapt to the situation.”
A small yet problematic laryngeal cleft
Maeve’s parents and her care team at Boston Children’s continued looking for answers. Despite regular therapy through the Feeding and Swallowing Program, she would still choke during swallow tests. But the Lee family remained confident. “We always believed her doctors would eventually diagnose her condition,” says Annemarie.
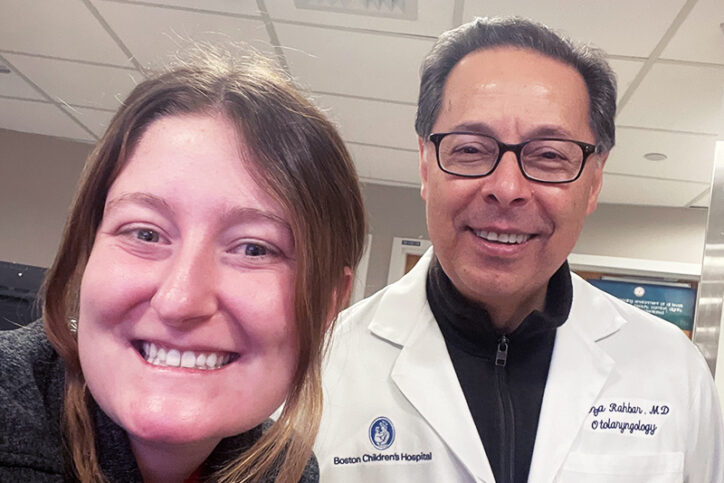
Dr. Bousvaros connected the family with his colleague Dr. Reza Rahbar, who is now director of the Center for Airway Disorders. He ordered a laryngoscopy and a bronchoscopy, which revealed that Maeve had a rare condition called laryngeal cleft. Hers was a type 1 laryngeal cleft, the smallest and therefore, most difficult type to detect.
In the early 2000s, few doctors knew about laryngeal clefts, an abnormal opening between the larynx (voice box) and esophagus. This can cause food and liquid to pass into the lungs, a problem called aspiration. Children with laryngeal cleft often have eating and breathing problems, including dysphagia (difficulty swallowing).

Some laryngeal clefts can be treated with feeding therapy. But by then, it was clear Maeve needed more aggressive treatment. Luckily, her diagnosis coincided with advances in surgical repair. Dr. Rahbar was one of a handful of surgeons performing minimally invasive endoscopic surgery to repair type 1 and type 2 laryngeal clefts at that time.
Maeve had the surgery when she was 5 years old. She, and other patients like her, are living proof that this approach, repairing laryngeal cleft endoscopically without any external skin incisions, leads to shorter hospital stays and less pain.
Maeve’s childhood with doughnuts and two belly buttons
“The first thing I asked for when I woke up from surgery was a honey-dipped doughnut,” says Maeve. It took some time to develop her swallowing muscles and eat without coughing, but soon she was eating whatever she wanted. It was the start of what she looks back on today as her normal childhood.
Her experiences did produce a memorable nickname: “double buttons.” Her older sister came up with the name when she saw the indentation left by the G-tube over her belly button.
And the nurses at Boston Children’s left another lasting impression. “They were so caring and compassionate,” says Maeve. “They’re the reason I became a nurse.”
From bed to the bedside
Today, Maeve knows what it’s like to be both a patient and a nurse. She can naturally empathize when patients struggle with the physical and emotional impact of feeding difficulty and aspiration. Hearing her early childhood story seems to help them see a more positive future for themselves.
One patient in particular stands out in her mind: a young boy with a G-tube. When he heard Maeve’s story, he became excited and said he’d never met anyone else like him. “He too had an amazing story,” she says. “And we were able to bond over our ‘second belly buttons!’”
Learn more about the Center for Airway Disorders.
Related Posts :
-

‘Sami’s trach helps him breathe’: Living with laryngeal cleft
Today, Sami is a playful toddler with so much energy that his parents need to remind him to take breaks. ...
-

Life-changing second opinion for laryngeal cleft helps Tyler thrive
When Brittany Browne was in school to become a speech language pathologist, she briefly learned about a type of congenital ...
-

Bringing Brazilian flair to blended diets: Josue’s g-tube journey
Josue Oliveira loves mealtime. In his large family — he’s the youngest of five kids — that means gathering around the ...
-

Taking charge: Emma perseveres with laryngeal cleft
Emma Morris is “a pistol,” says her mother, Sarah. “She’s a spitfire, passionate and caring.” But the 11-year-old gets ...





