Skin organoid could guide new treatments for skin conditions, hair loss
What does it take to build healthy skin? Two research groups converged on this question from different angles. They’ve now produced the most detailed view to date of the cell types and cell collaborations that go into creating our body’s largest organ.
Several years ago, Karl Koehler, PhD, and colleagues at Boston Children’s Hospital used pluripotent stem cells to create mini-organs (organoids) that capture most of the features of human skin, down to hair and hair follicles. Separately, researchers at the Wellcome Sanger Institute had been studying prenatal skin samples.
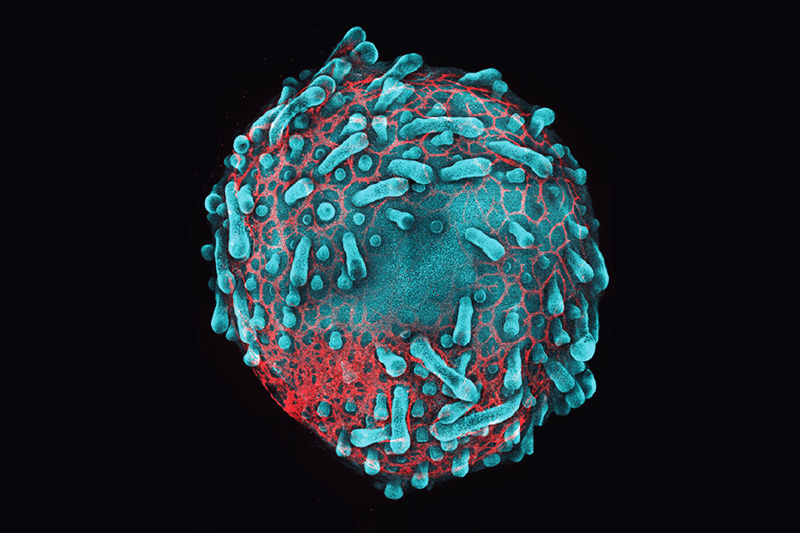
Teaming up, the two groups used single-cell sequencing and other genomic techniques to create a comprehensive cellular atlas of developing skin. They used the findings to refine the Koehler lab’s organoids.
The research, published in the journal Nature, could have many applications — from growing new skin to preventing scarring after surgery to regenerating hair after hair loss. Most immediately, Koehler wants to find treatments for genetic hair and skin disorders, particularly epidermolysis bullosa, a painful condition that makes skin fragile and prone to blistering and tearing.
“We can now leverage this atlas to learn to make better skin in a dish to model congenital disorders and develop gene therapies,” says Koehler, who co-led the new work with Sarah Teichmann, PhD, and Muzlifah Haniffa, PhD, at Wellcome Sanger. “That’s work that’s just getting going in our lab.”
Immune cells help organize developing skin
Some findings surprised the scientists. For example, it was known that macrophages — cells in the innate immune system — are present in our skin before we’re born, helping protect against viruses and bacteria. This study reveals that macrophages are also instrumental in the formation of skin tissue, vacuuming up cellular debris, helping repair wounds without forming scars, and refining the networks of blood vessels in the skin. That last role could help surgeons provide a more robust blood supply for skin grafts.
“When we included macrophages in our organoids, we saw much better blood vessels developing,” Koehler says. “Macrophages seem to have a role in building the architecture of the tissue.”
Further studies with the new organoids might also reveal why fetal and newborn skin heal much better than adult skin, without scarring, says Koehler. This could be key to regenerative medicine approaches.
From inner ear models to skin organoids
Strangely enough, Koehler began studying skin as an offshoot of his original work in the otolaryngology department at Boston Children’s, developing models of the inner ear. (Notably, the inner ear has something analogous to hair: tiny hair cells that, when vibrated by incoming sound waves, convert the mechanical waves into electrical signals that talk to the brain.)
“The skin and the inner ear are intimately related during development; the inner ear kind of buds off the skin,” says Koehler.
Sometimes in his experiments, he would inadvertently grow skin. That “pesky weed” in his cultures became a second focus of his lab, which is also affiliated with the Department of Plastic and Oral Surgery. “Sometimes I choose the project,” he says, “and sometimes the project chooses me.”
Visit the Koehler Lab and subscribe to our monthly research newsletter.
Related Posts :
-

Creating hairy human skin: Not as easy as you think
Key takeaways· Scientists have created the first cultured human skin capable of growing hair embedded ...
-

Microvillus inclusion disease: From organoids to new treatments
Microvillus inclusion disease (MVID) is a rare type of congenital enteropathy in infants that causes devastating diarrhea and an inability ...
-

Lung 'organoids' capture early-stage lung cancer; could help test treatments
Lung cancer, the leading cancer killer in the U.S., is often missed in its earlier stages. And while recent ...
-

Perfecting the craft of modeling disease in stem cells: Dosh Whye
Part of an ongoing series profiling researchers at Boston Children’s Hospital. Dosh Whye has always wanted to make peoples’ ...