Can we prevent leukemia in patients with Shwachman-Diamond syndrome?

Anna Nazarenko doesn’t see herself as sick. The strong-willed, spunky 6-year-old loves to dance and ski, and spent much of April Fool’s day pranking her parents. Aside from the enzymes she takes to help digest her food, you wouldn’t know that she has Shwachman-Diamond syndrome (SDS).
The rare, inherited type of bone marrow failure has also left Anna unable to make enough white blood cells. Infections are always a risk, and she may someday need a bone marrow transplant. But what Anna’s parents fear most is leukemia. For reasons that haven’t been clear, SDS seems to predispose children to this blood cancer.
Anna’s hematologist Akiko Shimamura, MD, PhD, directs the Bone Marrow Failure and Myelodysplastic Syndrome Program at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center. She is one of a just handful of people in the world studying SDS and its complications.
“Once patients with SDS develop leukemia, the prognosis is poor,” she says. “The best chance of prolonging survival is to intervene before the leukemia starts.”
Catching leukemia before it starts
Most children with SDS, including Anna, are born with a mutation in the SBDS gene. But over time, additional mutations tend to arise in their bone marrow. In work published recently in Nature Communications, Shimamura has pinpointed the specific changes that lead to leukemia, and now hopes to find ways to counter them.

In 2009, Shimamura launched a national patient registry for SDS. She has painstakingly gathered patients’ marrow samples and clinical data ever since, often working nights and weekends. The registry includes samples from Anna and has grown into a collaborative effort with colleagues at Cincinnati Children’s Hospital.
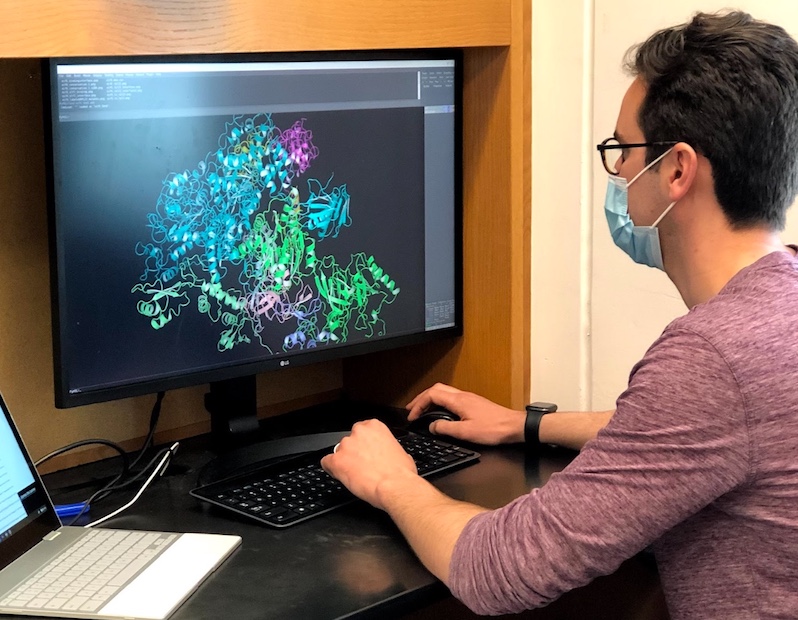
As genomics technology has advanced, the effort has paid off. Sequencing DNA from patients’ bone marrow cells collected year by year, Shimamura, with Alyssa Kennedy, MD, PhD, and Coleman Lindsley, MD, PhD, at Dana-Farber Cancer Institute and others, was able to track new mutations as they arose.
“We revealed some of the processes by which leukemia predisposition evolves,” she says. “This gives us a therapeutic target for intervention.”
Beyond SDS, the work could inform the development of treatments for children with a variety of leukemia predisposition syndromes. These include a long list of bone marrow failure disorders such as Fanconi anemia, Li Fraumeni syndrome, and congenital neutropenia.
Loss of p53
In the 110 registry patients Shimamura’s team studied, two mutations correlated with leukemia. One was in the TP53 gene well known to protect against cancer; its corresponding p53 protein is often called the “guardian of the genome.” However, leukemia developed if both copies of TP53 were mutated.
More on cancer predisposition genes
Two related studies from Dana-Farber/Boston Children’s looked at preventing leukemia by preventing a genetic “second hit” and at the possibility of adding a panel of cancer predisposition genes to newborn “heel stick” screening.
“We saw TP53 mutations arising frequently in the absence of malignancy and persisting for years,” says Shimamura. “Some patients developed as many as a dozen different TP53 mutations, yet remained stable. We were able to show that these stable patients had only one copy of TP53 knocked out, whereas those with leukemia had both copies knocked out.”
The recently developed technology of single-cell sequencing was critical to this discovery. Typically, DNA is sequenced for whole groups of cells at a time. But that technique misses genetic differences between cells.
“If we have a tube of cells and find two TP53 mutations, the mutations could both be in one cell, or each mutation could be in a different cell,” Shimamura explains. “You can’t say what’s happening on an individual cell level.”
She and her colleagues are now investigating strategies to screen for patients with a double TP53 hit, who would merit close monitoring for leukemia and possibly a bone marrow transplant.
“The results also suggest that a single-copy TP53 mutation as an isolated finding is not a reason to take a patient with SDS to transplant,” Shimamura adds.
Protective mutations
Mutations in a second gene, EIF6, were also common in patients with SDS. As with TP53, some patients acquired multiple different EIF6 mutations over time.
These mutations made bone marrow cells more “fit” and better able to function, the team found — even overcoming the effects of the SBDS mutation causing SDS to begin with. That original SBDS mutation interferes with the proper assembly of ribosomes, the structures inside cells that build proteins. Without functional ribosomes, the bone marrow ultimately fails, leading to SDS.
But in experiments, when Shimamura’s team mutated and inactivated EIF6, the problem with ribosome assembly was improved. Moreover, blood cells with EIF6 mutations did not subsequently acquire TP53 mutations.
“We never saw leukemia in cells with EIF6 mutations,” Shimamura says. “We now want to study these mutations in more detail and see if targeting EIF6 could offer a potential therapeutic strategy to reduce leukemia risk and prevent severe bone marrow failure at the same time.”
Steering cell fate
Both TP53 and EIF6 mutations essentially changed the trajectory of bone marrow cells, in different ways. A double TP53 mutation made marrow cells and their offspring more malignant and leukemia-prone, while EIF6 mutations had the opposite effect, allowing newly healthier bone marrow cells to predominate.
Based on her findings, Shimamura hopes to develop medical interventions that would redirect patients’ bone marrow back to a more benign state, heading off leukemia.

Anna’s parents are supporting these efforts. Over the past three years, they have raised almost $50,000 for Shimamura’s research.
“What she does is such a niche area in hematology, and SDS research is extremely underfunded,” says Matthew, Anna’s father.
“We hope to provide options to both improve blood counts and prevent leukemia,” says Shimamura. “That’s why we’re so excited about this work. I want to give a big shout-out to the patients in the registry who have stuck with us and made these advances possible.”
Learn more about our Bone Marrow Failure Program.
Related Posts :
-

New research sheds light on the genetic roots of amblyopia
For decades, amblyopia has been considered a disorder primarily caused by abnormal visual experiences early in life. But new research ...
-

Thanks to Carter and his family, people are talking about spastic paraplegia
Nine-year-old Carter may be the most devoted — and popular — sports fan in his Connecticut town. “He loves all sports,” ...
-

Tough cookie: Steroid therapy helps Alessandra thrive with Diamond-Blackfan anemia
Two-year-old Alessandra is many things. She’s sweet, happy, curious, and, according to her parents, Ralph and Irma, a budding ...
-

A new druggable cancer target: RNA-binding proteins on the cell surface
In 2021, research led by Ryan Flynn, MD, PhD, and his mentor, Nobel laureate Carolyn Bertozzi, PhD, opened a new chapter ...





