Poverty associated with suicide risk in children and adolescents
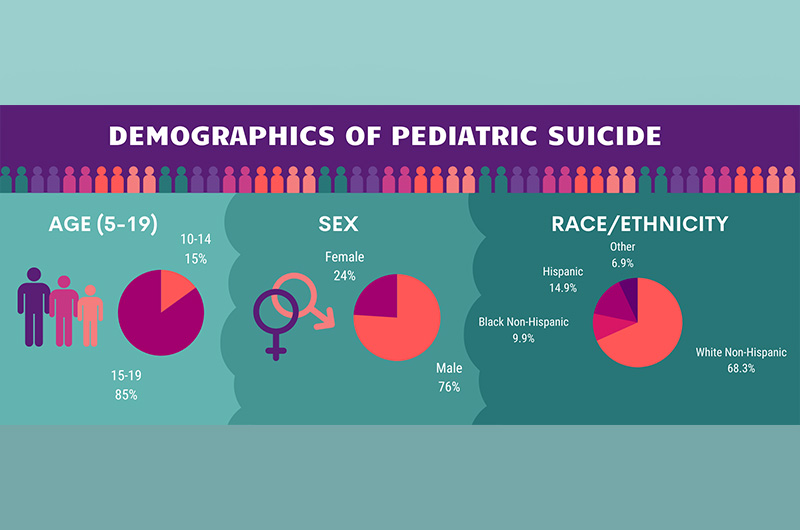
Suicide in children under age 20 has been increasing in the U.S., with rates almost doubling over the last decade. Between 2007 to 2016, nearly 21,000 children ages 5-19 years old died by suicide. While the reasons for the increase are not well understood, new research from Boston Children’s Hospital shows a link between poverty and suicide in children and teens nationwide.
The researchers grouped the number of suicides into five levels of poverty at the county level ranging from a low of 0-4.9 percent to greater than 20 percent. They learned that the rate of suicides in children and adolescents is 37 percent higher in counties with the highest levels of poverty – where more than 20 percent of the population in the county lives below the federal poverty level – compared with suicide rates in the lowest levels of poverty. The research was published in a paper in JAMA Pediatrics.
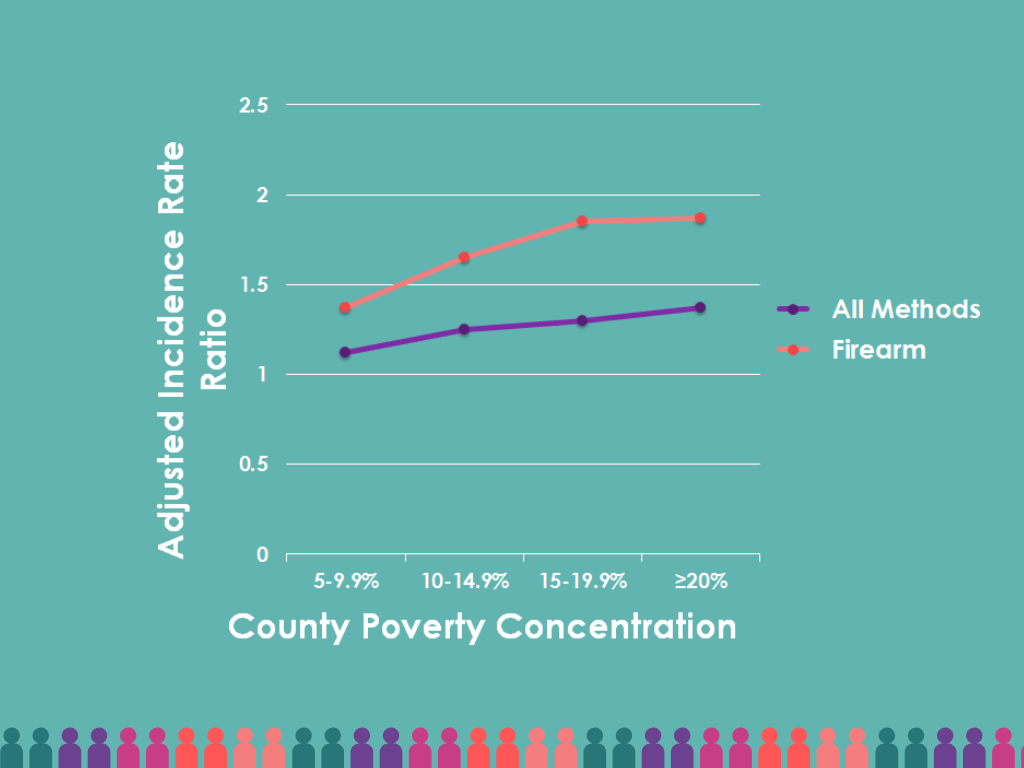
“The results were consistent in a step-wise fashion,” says Lois Lee, MD, MPH, of the department of emergency medicine at Boston Children’s Hospital. “As poverty increased, so did the rate of suicide.”

In this study, researchers collected information from the U.S. Centers for Disease Control and Prevention’s (CDC) Compressed Mortality File, which includes data on all U.S deaths., including cause of death. After searching for deaths by suicide, method of suicide, and county where the suicide occurred from 2007-2016, they paired that data with county-level poverty rates from US Census data and poverty estimates from the U.S. Census Bureau Small Area Income and Poverty Estimates (SAIPE) Program.
The findings from this study are similar to research from the CDC that found increases in suicide in youth and young adults ages 10-24 between 2000-2017.
Suicide by firearms linked with poverty
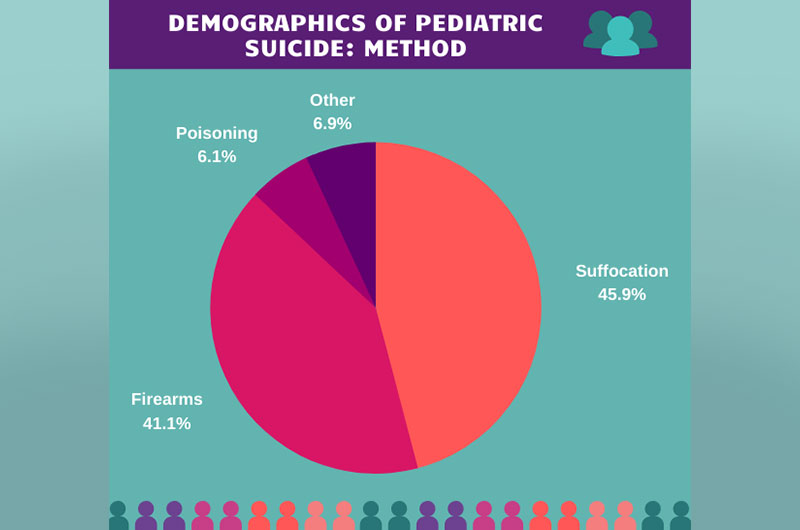
The study also revealed an increased suicide rate from firearms in the more impoverished counties compared to the least. However, suicide risk did not appear to increase for the methods of suffocation or poisoning – the two other leading causes of suicide in this study – based on county-level poverty. “This is important information since we know that firearm suicide attempts are far more lethal than other methods,” says Lee.
Lee and colleagues have been studying how poverty affects children’s health for several years. In an earlier paper, they discovered an increased risk of death for children < 5 years old from child abuse associated with counties with higher poverty levels. And in their own professional experience, they have seen a rise in the number of children and teens with mental health issues, including suicide attempts or thoughts of suicide, seeking care in the emergency department (ED). In a 2019 paper, they published research noting the rates of mental health visits in children ages 5-18 to the emergency room increased 5.5 percent annually from 2010-2016. Not only did the rates of mental health visits increase, but also the number of hours the patients were cared for in the ED. Mental health ED visits lasting more then 24 hours increased from 4.3 percent of mental health visits in 2010 to 18.8 percent of visits in 2016.
“From our knowledge about rising suicide rates in children and adolescents and how poverty influences childhood health, it was important to see if there was an association between the two,” Lee explains.
A window into suicide prevention
Knowing more about the associated risk factors for pediatric suicide may help guide interventions to prevent them.
“This study is more evidence that to provide the best healthcare for all children and youth, we need to try to improve some of the socio-economic areas or conditions where these children live,” says Lee. “At a minimum, that means actions like improving parental employment, increasing the minimum wage, and ensuring that everyone has health insurance.”
In recent years, research has been building that toxic stress during childhood has long-term health implications. “We know that adverse childhood experiences and toxic stress can affect behavioral and mental health,” says Lee. “It may also result in changes at the cellular level in the human body.”
The study authors report that children living in poverty are likely to be exposed to more family turmoil, violence, social isolation, and lack of positive peer-to-peer relationships and may be more likely to have emotional difficulties like depression and anxiety. Further, areas of concentrated poverty may lack infrastructure such as quality schools, sustainable jobs, health care facilities, and mental health resources supporting good health for adults and children.
Says Lee, “As pediatric suicide rates in the U.S. continue to rise, we must work to understand the contributors to pediatric suicide, including poverty-related factors, so that suicide prevention efforts can focus on the children at highest risk.”
Other contributors to this work are Jennifer A. Hoffmann, MD, formerly of BCH, now at Ann & Robert H. Lurie Children’s Hospital of Chicago and Caitlin A. Farrell, MD, Michael C. Monuteaux, ScD, and Eric W. Fleegler, MD, MPH, of Boston Children’s Hospital.
Related Posts :
-

A better treatment for endometriosis could lie in migraine medications
Endometriosis is a common, mysterious, often painful condition in which tissue similar to the uterine lining grows outside the uterus, ...
-

Status epilepticus: What’s changed, what to know, and a global perspective
Status epilepticus, or a prolonged seizure lasting more than five minutes, is a rare complication of epilepsy and a medical ...
-

Injected microbubbles could be a safe way to deliver emergency oxygen
For years, researchers and clinicians have been trying to find a way to rapidly deliver oxygen to patients when traditional ...
-

Emergency department or urgent clinic? Understanding your options if your child is injured
Having an active or adventurous child often means comforting them when they come home with bumps or bruises. But when ...





