Frozen poop pill offers a less invasive treatment option for emerging infectious disease
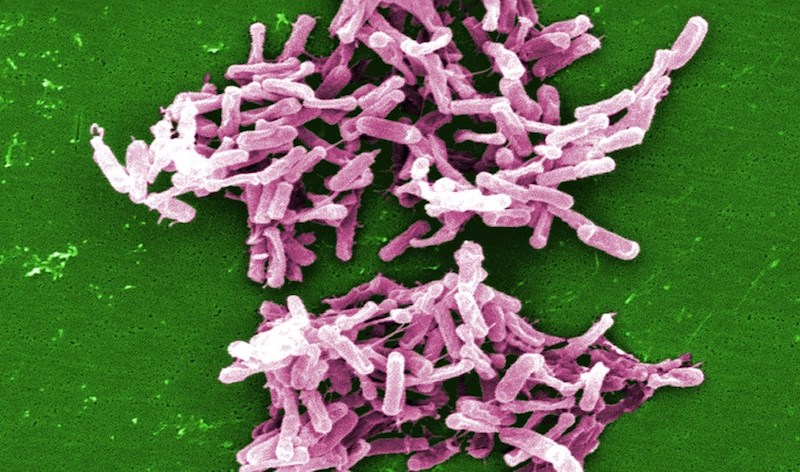
The fecal microbiota transplantation (FMT) movement is catching the attention of scientists, researchers and the media nationwide. Currently, fecal transplantation delivers pre-screened, healthy human donor stool to a patient via colonoscopy or by nasogastric tube. It’s prescribed as an effective alternative to long-term antibiotic use in treating debilitating infectious diseases such as Clostridium difficile, also known as C-diff.

But new research published in the Journal of the American Medical Association says there is a third, less invasive, less expensive option to treat C-diff: poop in a pill.
“This ground-breaking paper shows that with encapsulated, frozen donor stool, fecal transplantation can be used to successfully treat recurring C-diff infection in 90 percent of cases,” says George H. Russell, MD, MS, pediatric gastroenterologist in the Inflammatory Bowel Disease Center at Boston Children’s Hospital and co-author of the Massachusetts General Hospital-sponsored study. “[The study] provides proof-of-concept that invasive means do not need to be used to deliver the fecal transplant.”
Though the poop pill is still in the experimental therapy stage, Russell says this cutting-edge research is spurring further clinical research at Boston Children’s Hospital, specifically using fecal microbiota transplantation in other disease states, such as inflammatory bowel disease. The goal, he says, is to help push forward the development of marketable, encapsulated, healthy donor stool samples for patients with C-diff.
The changing pediatric C-diff climate
The Centers for Disease Control and Prevention identifies C-diff as a health care–associated infection—one that causes debilitating diarrhea and is linked to 14,000 American deaths annually.

Typically acquired in a hospital setting, pediatricians are seeing a surge in community-acquired C-diff where one would never expect to see it at all.
“This is an exploding problem in the pediatric population,” says Russell. “We are seeing kids coming in without exposures to a hospital environment who are getting C-diff infections.”
Treating C-diff begins with administering antibiotics. However, recurrence is likely. By the third recurrence, it is unlikely antibiotics will cure the infection, therefore, a fecal transplant may be considered, Russell says.
About the poop pill study
In the 2014 study, researchers from Massachusetts General Hospital, Boston Children’s Hospital, Harvard Medical School and Tel Aviv University evaluated 20 patients, ages 11 to 89, who had at least three episodes of recurrent C-diff infection.
Each patient consumed 15 stool capsules from pre-screened, healthy volunteer donors, over a two-day period. Diarrhea resolved in 14 of the 20 patients after the first treatment. The six non-responders were retreated, and four had resolution of diarrhea after their second treatment.
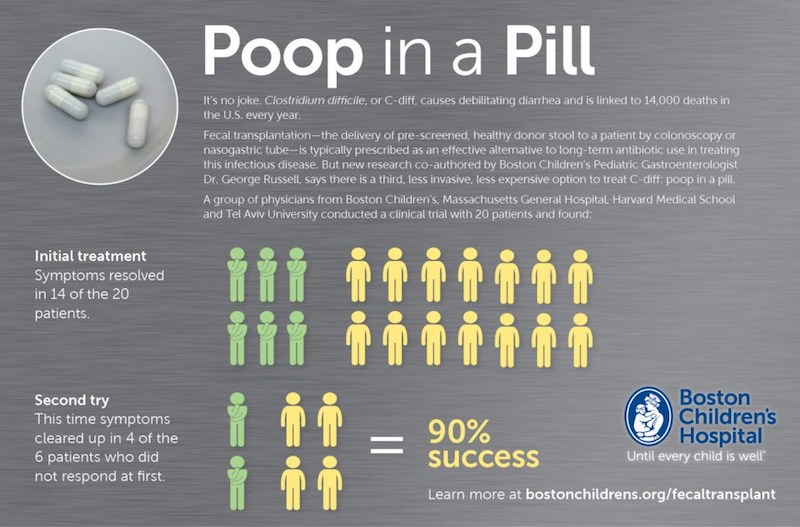
Overall, patients had fewer daily bowel movements and no relapses of diarrhea for eight weeks following treatment. The results of the study equate to a 90 percent success rate.
“The study showed you can use frozen donor stool successfully and safely, and it doesn’t matter how you deliver it—from above or below,” Russell says.
Homegrown poop pill is not an option
As fecal transplantation and frozen poop pill usage gain increased media attention, some people are self-prescribing homegrown poop pills.
Russell stresses that encapsulated, frozen stool is an experimental therapy and must be administered by a health care professional—preferably one who is sharing and collecting this data with the FDA and following established scientific protocols. “This is a safety concern, and that is why the FDA has mandated it is only appropriate for a licensed practitioner to administer the treatment,” he says.
For the future
Russell says the poop pill has vast potential. Based on this potential, he and other researchers are continuing to explore how fecal transplantation might be used to treat other GI conditions such as Crohn’s disease and ulcerative colitis.
“We know there is dysbiosis [imbalance] in the gut with inflammatory bowel disease patients,” says Russell. “We have actively applied to the FDA to look at treating active ulcerative colitis and Crohn’s with FMT to see if it makes a difference in their clinical course and reduces need for immunosuppressive medications.”
Related Posts :
-

Team spirit: How working with an allergy psychologist got Amber back to cheering
A bubbly high schooler with lots of friends and a passion for competitive cheerleading: On the surface, Amber’s life ...
-

Thanks to Carter and his family, people are talking about spastic paraplegia
Nine-year-old Carter may be the most devoted — and popular — sports fan in his Connecticut town. “He loves all sports,” ...
-

No limitations: How Flora found answers for MOG antibody disease
Flora Ringler’s fifth birthday didn’t turn out as she had hoped. She and her family were vacationing in ...
-

Genetic causes of congenital diarrhea and enteropathy come into focus
Congenital diarrheas and enteropathies are rare and devastating for infants and children. Treatments have consisted mainly of fluid and nutritional ...





