Culture shock: Why poliovirus had to live before it could die
Today, stories of polio may seem like echoes from far-away history to those born after 1979, the year that polio was eradicated in the U.S. Since then, it has been customary for children to receive four doses of the polio vaccine to protect them from ever contracting the terrifying disease also known as “infantile paralysis.”
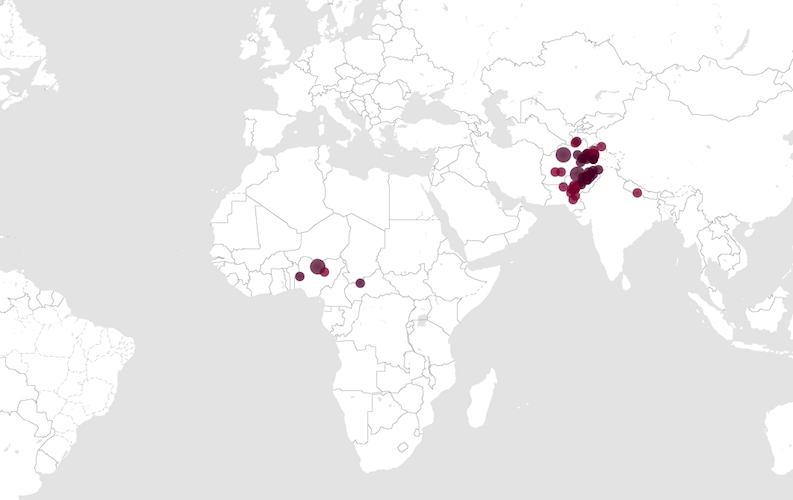
Polio, however, still afflicts people in some areas of the world today. It causes muscle wasting and — in the most severe cases — can completely rob a person of his or her ability to move or breathe, resulting in death.
In the U.S., research efforts to create a polio vaccine lasted much of the 20th century. Although the virus was thriving and spreading among people, researchers repeatedly failed at getting poliovirus to survive in culture.
Then, one of the most crucial breaks in the fight against polio occurred in a Boston Children’s Hospital laboratory in 1949, during the heyday of polio outbreaks. Three Boston Children’s scientists researching a whole host of diseases including mumps, influenza and chicken pox managed — unintentionally, ironically enough— to discover the first reliable method for culturing poliovirus in human skin and muscle cells. Their findings opened the door for development of the Salk and Sabin polio vaccines that would deliver the U.S. from the grips of polio.
A 40-year battle against polio
Starting back in 1916, polio infection was on the rise. That year, Boston Children’s admitted 165 children with paralysis caused by polio. The viral infection was unpredictable and mysterious. Its spread seemed to spike during the summer months. How it transmitted from one person to the next was not yet understood.

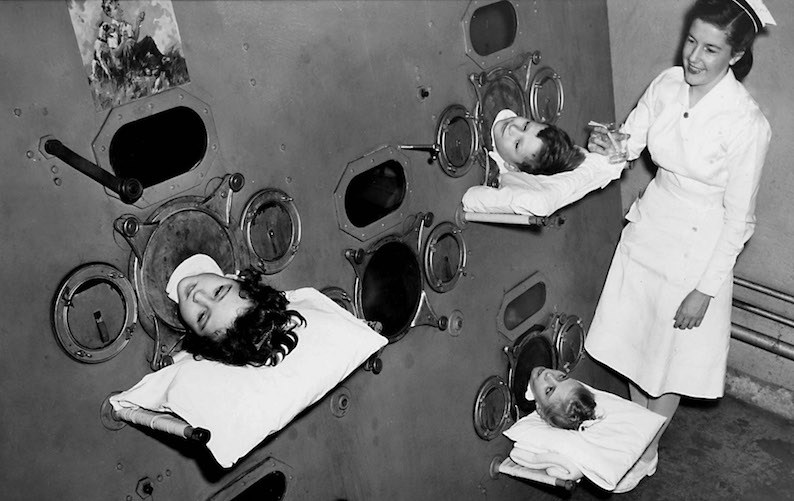
While some children never developed any symptoms of having polio, others became partially or totally paralyzed. Afterwards, some never recovered their lost muscle function. For those who became so weak they could no longer breathe on their own, iron lungs gave them their breath at the cost of living inside the machine from the neck down. For others, even an iron lung’s breathing assistance could not overcome the effects of respiratory muscle paralysis. Treating polio patients from all over New England, Boston Children’s became headquarters for the Massachusetts Infantile Paralysis Commission.
But the 1916 outbreak was just the beginning. Over the next 40 years, generations of parents lived with the fear that their children would get polio. Annual epidemics in the U.S. became more and more severe. During the late 1940s to the early 1950s, the Centers for Disease Control and Prevention (CDC) estimate that polio paralyzed around 35,000 people each year.
The dream of making a vaccine from poliovirus
At Boston Children’s, responding to polio epidemics had become the new normal. Polio paralysis was responsible for more orthopedics cases than any other disease or condition.
Researchers all over the country spent year after year trying to learn as much as possible about poliovirus in hopes that they could develop a vaccine against it. To do so, they needed to find a way to culture and isolate the virus.
In 1936, the first dash of hope came from a laboratory in New York. Scientists at the Rockefeller Institute had learned to culture poliovirus in human nerve cells. However, they worried that developing a vaccine using nerve cells could jeopardize the central nervous systems of those who were vaccinated.
So, scientists marched on. It would be a dozen more years before fortunate happenstance — as so often occurs in trial-and-error research — cleared a path forward for polio vaccines.
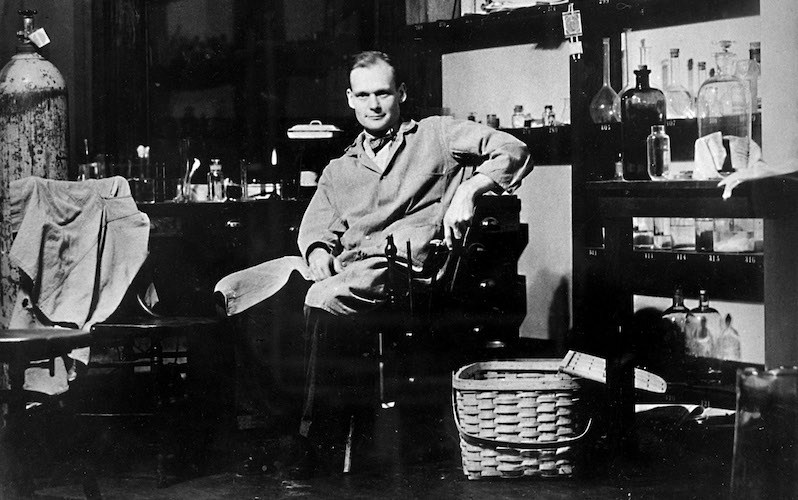
At long last, a group of researchers in the Enders lab at Boston Children’s – including John F. Enders, Thomas H. Weller and Frederick C. Robbins — unveiled a method for culturing poliovirus in a variety of human skin and muscle tissue samples. These types of cultures were considered a safer route for developing vaccines than using nerve cells.
The milestone achievement by the Enders lab had actually happened quite serendipitously. While attempting to culture chicken pox, the researchers used poliovirus to inoculate a control group of tissue samples. Unexpectedly, their method was well-suited to growing poliovirus instead of chicken pox. The chicken pox failure was a landslide success for polio vaccines. Their celebrated work was published in Science in 1949.
Polio vaccines arrive amidst Massachusetts outbreak
After the Enders lab announced their method for culturing poliovirus, scientists everywhere began working at a breakneck pace to develop vaccines against polio. Two leaders on this front quickly emerged. Jonas Salk, a researcher at University of Pittsburgh, used inactivated poliovirus to develop an injectable vaccine. Albert Sabin, a researcher at Cincinnati Children’s Hospital, developed an oral vaccine that used weakened, live poliovirus.
In our labs, the increasing war on the virus will continue ~ P.D. Howe, 1955
In the 1950s, various versions of the Salk and Sabin vaccines began undergoing analysis and subsequent clinical trials amid much excitement. In 1955, the same year that the Salk virus became available to the public, the polio epidemic reached a most-feverish pitch in Boston. More than 650 new polio patients were admitted to Boston Children’s that summer.
Throughout the 1955 epidemic, practically all of Boston Children’s wards were dedicated to treating polio patients, with nurses and doctors working extraordinary around-the-clock shifts. In August 1955, the number of patients in the hospital rose above what was considered the maximum possible, with 66 percent of all patients at the hospital receiving treatment for polio.
A polio-free world in sight
Although the timing of the massive outbreak was disheartening, the scientific and medical community remained optimistic that the new polio vaccines would soon take effect.
Amidst the 1955 crisis, then-president P. D. Howe wrote, “The achievements of Dr. Enders and his colleagues put eventual control [over the spread of polio] in our grasp. It is a sorry coincidence that in this, the first year of an anti-polio vaccine, we should experience a regional epidemic.”
Howe’s prediction turned out to be rather prophetic. By the end of the 1950’s, polio did finally come under control thanks to widespread immunization using the Salk and Sabin vaccines. For their contributions that enabled the vaccines to be developed, Enders and his team received the 1954 Nobel Prize in Physiology or Medicine.
Since 1979, no new cases of polio have originated in the United States, according to the CDC. Enders passed away in 1985 at the age of 88, having lived long enough to see the rise and fall of polio’s spread in the U.S.
Looking to the future, international health organizations have formed the Global Polio Eradication Initiative to strategically make sure that all children, through effective vaccination, have the opportunity to live their lives without fear of contracting polio. That plan, set in motion in 2013, is striving to see the world be polio-free by 2018.
Related Posts :
-

Building better antibodies, curbing autoimmunity: New insights on B cells
When we’re vaccinated or exposed to an infection, our B cells spring into action, churning out antibodies that are ...
-

Could SIDS be caused by unrecognized brain infections?
Some infants who pass away from sudden infant death syndrome (SIDS) are known to have had acute minor infections. Could ...
-

Could a GI bug’s toxin curb hard-to-treat breast cancer?
Clostridium difficile can cause devastating inflammatory gastrointestinal infections, with much of the damage inflicted by a toxin the bug produces. ...
-

A new approach to C. diff? Targeting the inflammation, not the bacteria
Clostridium difficile (C. diff) intestinal infections can cause severe, debilitating diarrhea in patients who are hospitalized or on immunosuppressive therapies. ...





