New technique designed specifically for children gives surgeons another moyamoya treatment option
Moyamoya is rare blood vessel condition that is a major cause of pediatric stroke. Surgical revascularization can be very effective; however, anterior cerebral territory ischemia can occur after treatment, particularly in children with delayed disease progression.
The current surgical treatments for anterior cerebral territory ischemia in pediatric patients are challenging: Complex, high-risk procedures haven’t been well studied in this population and burr holes, while technically simpler, have limited efficacy in children older than infants.
PiPed for anterior cerebral territory ischemia
To address this problem, Edward R. Smith, MD, Darren B. Orbach, MD, PhD, and their colleagues in the Cerebrovascular Surgery and Interventions Center at Boston Children’s Hospital developed a surgical approach to revascularization in these patients. Specifically, they sought to create a technique that was both lower risk than complex approaches adapted from adult populations, but more effective than simple burr holes.
Known as pial pericranial dural (PiPeD) revascularization, this technique builds on the principles of pial synangiosis, a procedure that reroutes the healthy scalp blood vessel to the brain, bypassing the narrowed vessels. Although pial synangiosis is an option when an adequate vessel is located over the area of ischemia, no adequate blood vessel is available in some cases.
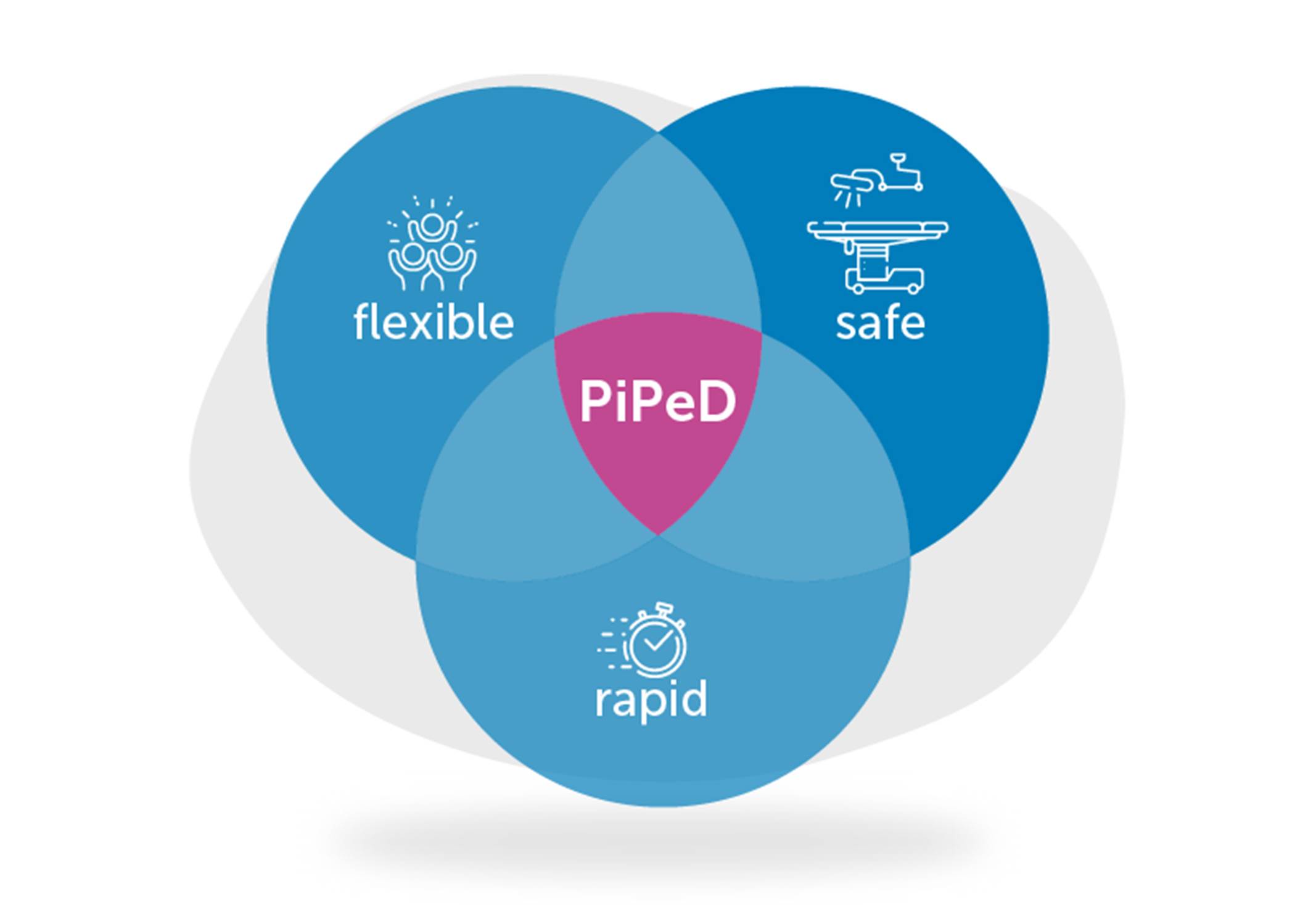
PiPeD offers surgeons another choice by using the pericranium and dura — rather than a distinct vessel — as the primary vascular supply and involves a larger craniotomy with arachnoid dissection. This provides robust full-territory revascularization in children of all ages — and is less risky than more complex procures.
“We designed this approach based on the principles of Dr. R. Michael Scott, who developed the moyamoya practice at Boston Children’s, and sought to incorporate the knowledge learned from hundreds of operations studied over decades,” says Smith.
A new tool for physicians
The team reviewed records from 21 Boston Children’s moyamoya patients who had undergone PiPeD for anterior cerebral territory ischemia. They found that the use of dura and pericranium for indirect revascularization provided robust vascularized graft with great flexibility in location and high potential for engraftment: After an average of about two years, radiographic engraftment was present in nearly 91 percent of patients. In addition, the patients had experienced no new strokes, even when their disease had progressed.
The findings of this study were published in the July 2, 2021, issue of the Journal of Neurosurgery: Pediatrics.
“This surgery combines the rapid and safe parts of indirect grafting, while allowing a remarkable flexibility to treat nearly any child, regardless of previous surgeries or location of possible arteries — a big advance over other methods and a powerful new tool to help protect children from stroke,” says Smith.
Learn more about the Cerebrovascular Surgery and Interventions Center or refer a patient.
Related Posts :
-

Groundbreaking research identifies noninvasive biomarker for moyamoya in children
Moyamoya is a rare blood vessel condition that has an outsized impact on children, as it is responsible for about 6 ...
-

Another shot for Conner: Getting back in the game after brain surgery
Watch Conner Hicks coach basketball at Midlakes Middle School in Clifton Springs, New York, and you’ll see a young ...
-

Advice for moyamoya families from a mom who’s been there
About a year ago, our 4-year-old daughter, Kalea, started having headaches. After four months, we called our pediatrician because the ...
-

When surgery shapes your life: Moyamoya patient turned doctor
Elizabeth Kwak is living proof of how far the treatment of moyamoya has come. Twenty-four years ago, Elizabeth had pial ...





