Hemophilia A gene therapy paves the way for a life with less pain

Matthew Harrington, a 35-year-old oil-field worker from Douglas, Wyoming, knows pain.
Born with hemophilia A, a rare condition in which the blood doesn’t clot properly, Matt’s body — both inside and outside — has difficulty stopping bleeding. He has what’s considered the most severe form of hemophilia, characterized by frequent bleeding episodes, particularly in the muscles and joints.
“It’s extremely painful, like spraining your ankle and having someone grab it and squeeze it every 30 seconds,” he says.
Hemophilia A is caused by a mutation in the F8 gene that leads to low levels of factor VIII (8), a protein necessary for clotting. Normal ranges for factor VIII levels are 50 to 150 percent. Matt’s is less than 1.
“For individuals like Matt with severe hemophilia A, even the slightest injury — bumping the counter, tripping on the stairs, or just sitting on the couch — can result in prolonged or spontaneous bleeding,” says Dr. Stacy Croteau, director of the Boston Hemophilia Center, a joint program between Dana-Farber/Boston Children’s Cancer and Blood Disorders Center and Brigham Health. “It really has a substantial impact on day-to-day life.”

Growing up with hemophilia A
As far back as Matt can remember, he has needed regular intravenous (IV) infusions of factor replacement to prevent bleeding episodes. This current standard-of-care treatment is cumbersome in any situation, but for a young boy growing up on a ranch, it was a heavy burden.
“When I was a kid, we were always riding horses or dirt bikes, and I loved sports, but as a hemophiliac you’re not made for any of that stuff really.”
Matt would get regular joint bleeds in his ankles and his mom would rush him to the emergency room so he could get infused, and then he’d be out of school for several days. “This went on and on,” he says.
As an adult, navigating chronic pain was part of Matt’s everyday routine. The physical grind of working in the oil fields had begun to take its toll.
“Throughout the night, I would wake up with my ankles throbbing. And the next day, I would be so stiff I couldn’t walk. I’d literally crawl to the bathroom to soak my ankles for 45 minutes before I could even begin to start my day. It was wearing me out.”

From chronic pain to pain free
In March of 2019, Matt and his family traveled to Massachusetts to participate in a gene therapy clinical trial for hemophilia A. Led at Boston Children’s by Dr. Croteau, the goal of the trial is to boost production of the missing or abnormal clotting factor, and reduce — or hopefully eliminate — the need for factor replacement therapy.
Matt’s sister had discovered information about the trial online, and he was fortunate to meet the criteria. “I thought, what do I have to lose? I’ll give it a shot.”
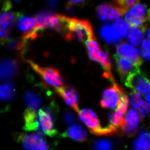
On an early spring morning, Matt and his wife arrived at the Boston Children’s Experimental Therapeutics Unit. He says the process was far more simplistic than he imagined. He lay on a hospital bed with a tiny bag of clear fluid hooked up to his IV. During the short IV infusion, a genetically engineered carrier, called a vector, delivered a functional copy of the F8 gene. Only one dose was needed.
“When you hear gene therapy, you might imagine a complicated or invasive procedure to manipulate all kinds of cells and DNA in the body,” says Dr. Croteau. “But in some ways, the treatment is anticlimactic because it’s just an IV infusion, yet as a novel therapy still has the feeling of something really magical.”
Learn how gene therapy for Hemophila A works.
Matt and his wife flew home the next day. Three days later, Matt traveled to the high mountain streams and big boulders of Northern Idaho for a steelhead fishing trip with his brother. He joyously jumped from rock to rock — something he couldn’t normally do prior to gene therapy. That night, he recalls lying in bed and suddenly realizing he was no longer in pain.
“I felt normal,” he says. “There was no throbbing, no bruising. There was nothing. And the next morning, I got out of bed, and I actually walked to the kitchen to make coffee. It was unreal.”
Even Dr. Croteau was surprised by Matt’s rapid and positive response. “It’s just such a success whenever you have the good fortune to be able to share a treatment with someone that really makes their life better and not only better, but easier. It’s a huge win.”

What does the future hold?
Dr. Croteau notes that each individual responds differently to gene therapy; the magnitude (measurable factor levels), timing, and durability of response is broad. For Matt, his levels are now in the mild hemophilia range — a dramatic improvement from his severe disease, not only in terms of his improved laboratory results, but also in his everyday life, and ability to enjoy his family and favorite activities.
“Although he isn’t above 50 percent — the cutoff for normal — getting into the mild hemophilia range makes a big difference in terms of how a patient feels and how likely they are to have bleeding with minor injury.”
The data that’s been presented for multiple gene therapy programs, especially the ones currently enrolling, show that most participants have some response. Yet, Dr. Croteau remains cautiously optimistic. “It’s still too early to make any guarantees, but we are confident and hopeful.”
A year and a half after gene therapy, Matt is still jumping rocks and in awe of his miraculous transformation. “My life is changed,” he says. “I no longer require [regular or frequent] factor replacement. I never even think about hemophilia. It’s just awesome.”
Learn more about the Gene Therapy Program.
Related Posts :
-

Accessing hemophilia care: A tale of two countries
When Miguel and Marco Antonio were born in the Philippines, they had a 50 percent chance of having hemophilia, as two ...
-

An education in hemophilia for Colin’s new school
Every morning, one of Colin Bazinsky’s parents puts a needle into his chest to give him an infusion of ...
-

Breaking gender biases: What is it like to be a girl with severe hemophilia?
In human biology class this past semester, Morgan DiPrima viewed a PowerPoint presentation that made her head spin. It included ...
-

Long-term hemophilia treatment could lie in patients' own cells
Children (and adults) with hemophilia are slow to form blood clots, so are at constant risk for uncontrolled bleeding. Even ...