Healing the heart, mind, and spirit

For most of her life, Siena Tancredi worried about her heart beating too fast.
She has long QT syndrome, an inherited condition that affects the heart’s electrical rhythm and can cause fast, erratic heartbeats. From the time she was diagnosed at age 10 and into adulthood, she avoided any situation that would potentially cause her heart to race. Underlying her concern was the painful memory of how long QT syndrome caused the death of her 14-year-old brother, Skylar, while they swam together.
“I had gone through most of my life being told if you strenuously exercise, you increase the risk of cardiac arrest and death,” says Siena, 27. “I always thought my heart rate couldn’t be above 130 beats per minute because that was my threshold of safety.”
Caution often led to paralyzing fears. By last year, Siena faced several health issues that she connected to long QT syndrome. She came to Boston Children’s expecting help for her heart —but she got more than that. Siena’s participation in the hospital’s Cardiac Fitness Program led her to realize, like many other patients, what she really needed was treatment for the heart, mind, and spirit.
Connecting the heart and brain to overall health
Siena’s treatment involved only an exercise program, but many patients with structural congenital heart defects (CHD) need more extensive care for their heart and neurodevelopment. There are many factors that create that need but they include genetic changes to the heart as well as changes to how the brain develops in utero, says Dr. Caitlin Rollins, director of Boston Children’s Cardiac Neurodevelopmental Program. CHD, for example, can affect development of the placenta and how it delivers nutrients and oxygen to the fetal brain. Children who have repeated surgeries for heart defects are also at risk of brain injury.
With volumes of research detailing how children with CHD are at increased risk for neurodevelopment impairments — including developmental delay, motor concerns, attention deficit hyperactivity disorder (ADHD), and learning disabilities — heart clinicians, neurologists, and rehabilitation specialists recognize the importance of working together to coordinate care. “The heart and the brain are so interrelated that it’s a core part of congenital heart disease management,” Rollins says. “That’s why cardiologists will talk to families about how school is going and their child’s development.”
When children recover from heart treatment, they can get help with developmental, behavioral, and learning challenges. Children and adults can also learn to safely push their whole selves through cardio fitness, as Siena did. These efforts improve not just neurodevelopment and cardiovascular health but also overall wellbeing and confidence.
“A child who has a heart condition and gross motor delay can make tremendous gains through physical therapy,” Rollins says. “As some children age, some cognitive issues might remain, but even then, we can help them learn strategies to compensate for areas where they are weaker — maybe it’s medication or accommodations at school. When they have support, it can have a wonderful effect on their confidence and what they’re able to accomplish.”
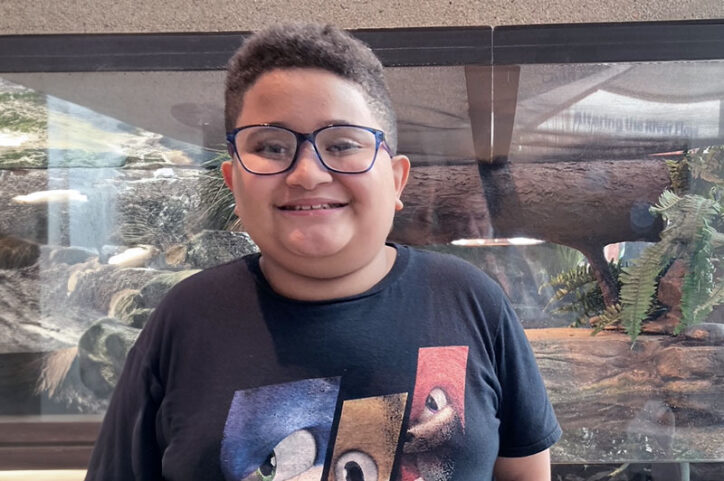
Isaiah hits his stride at school and in life
Isaiah Jackson is one of those children. He was born with transposition of the great arteries (TGA). His aorta and pulmonary artery were reversed from their typical positions in the heart anatomy, making his blood circulate in the opposite direction. Not long after birth, he had cardiac catheterization and “arterial switch” surgery at Boston Children’s to connect the aorta and pulmonary artery to their proper ventricles.
But it didn’t take long for Isaiah’s mother, Michelle, to notice the signs of a likely connection between his CHD and neurodevelopment. As an infant, he couldn’t hold his toys, and when he learned to walk, he did so with slight difficulty. He also had trouble speaking.
Isaiah returned to Boston Children’s, this time to work with specialists from the Cardiac Neurodevelopment and Augmentative Communication programs. They helped improve his fine motor skills and speech. Later, when he developed behavioral issues that carried over into school, the specialists helped place him in a school for children with moderate to severe disabilities.
Isaiah, now 11, has embraced his heart journey. “Before he was always self-conscious about his surgery scar,” Michelle recalls. “But now sometimes he’ll pull up his shirt and say, ‘This is my scar. I was born with a heart defect.’ He understands what it means.”

Atiana overcame major medical obstacles
Atiana Lancaster would get impatient with her rehabilitation, nearly a decade ago, from several cardiac arrests that were followed by brain injury. She felt frustrated when a doctor tested her mental recall with simple questions. “I thought it was pointless,” she recalls. But she would also get frustrated with herself when her mind couldn’t keep pace with her hands. “I had pretty handwriting before I got sick, but afterwards trying to learn how to hold a pencil was difficult, so were buttoning buttons, tying ties, and zippering zippers.”
Then 13, Atiana needed extensive physical and cognitive-speech rehabilitation. When her heart stopped beating during cardiac arrest, caused by the condition myocarditis, she was without oxygen for a considerable amount of time. She also received extracorporeal membrane oxygenation (ECMO) treatment at Boston Children’s. ECMO took over the work of her heart and lungs so they could heal, but it was apparent she would eventually need rehabilitation. Her medical team wasn’t initially sure if she would recover her cognitive abilities, speech, and motor function.
Dr. Ana Ubeda Tikkanen, a rehabilitation doctor at Boston Children’s Pediatric Rehabilitation Medicine Program and director of Cardiac Surgery’s rehabilitation program, specializes in helping children recover functionally and adjust to life after surgeries for CHD, heart transplants, and the implantation of heart pumping devices. She led Atiana’s rehabilitation team.
Learn how Atiana found inner strength to recover
“We break down rehabilitation into small steps,” Dr. Ubeda Tikkanen says. “One step might be a patient just getting up and dressing themselves. The next day it’s walking 300 feet. It’s about reaching short-term goals they can achieve, to prove to them they can keep advancing in the direction they want to go.”
Whenever Atiana hit a roadblock during occupational and physical therapy, she voiced her frustration and detailed what seemed insurmountable. Her therapists replied that her experience was normal for that stage of rehabilitation and urged her to keep practicing what was once routine so it could again be routine. She learned to focus on the finish line.
“People say you have to live in the moment, but if I lived in that moment, I don’t think I would have made it here — now being able to walk, talk, and do everything that I’m doing. Instead, I thought about my future.” That future is here. She now works as a phlebotomy specialist with the dream of someday becoming a nurse. She also enjoys traveling with her mom, Nicole.
After hitting a low point, Siena reached new heights
Siena can’t believe she is now jogging on a treadmill and playing pickleball. Last year, she couldn’t shake fatigue, and she fainted often. After consulting her cardiologist from her home state of New York, she was referred to Boston Children’s Center for Cardiovascular Genetics, where she saw cardiologist Dr. Elizabeth DeWitt. “It was a transformative appointment,” Siena recalls.
Dr. DeWitt found that Siena had a small atrial septal defect, a hole in the wall that separates the heart’s upper chambers, but it does not require surgical repair. Instead, Dr. DeWitt recommended that Siena exercise under the supervision of the Cardiac Fitness Program, which works with children and adults. “As someone who has had so much emotional trauma around exercise and movement, this was a way for me to be monitored with EKGs and vital checks so I could gain confidence,” says Siena, who now lives in Boston. “I can now live a normal, active life and be healthier mentally and physically.”
Dr. DeWitt told Siena the program could be life-changing. “It wasn’t until I was going several times a week and working closely with the staff that I realized she was right,” Siena says. “It changed the trajectory of my life. The function of my heart is not a worry every second of the day. It showed me what I’m capable of, and I owe it all to the cardiac team at Boston Children’s.”
Learn more about the Cardiac Fitness and Cardiac Neurodevelopmental programs.
Related Posts :
-

Whether she's embracing school, sports, or music, Lindsey shows how Williams syndrome can be managed
One of the first things Lindsey Franco will tell you is, “I like being me. I like being happy.” The 19...
-

Twenty years after a groundbreaking biventricular repair, Faith gives back by helping children with CHD
Faith Brackett doesn’t remember every detail of the time she was among the first children to have a new ...
-

A lifetime of treatment inspires Ruth to advocate care for others
Ruth Ngwaro offers guidance to children who have heart disease. Perhaps her most useful bit of advice is telling them ...
-

Treatment for a complex congenital heart defect gives Alyvia 'endless energy'
She may be just 3 years old, but Alyvia Parker is already making a difference for other kids with congenital ...





