Endocrine-oncology treatment helps teen with rare genetic condition
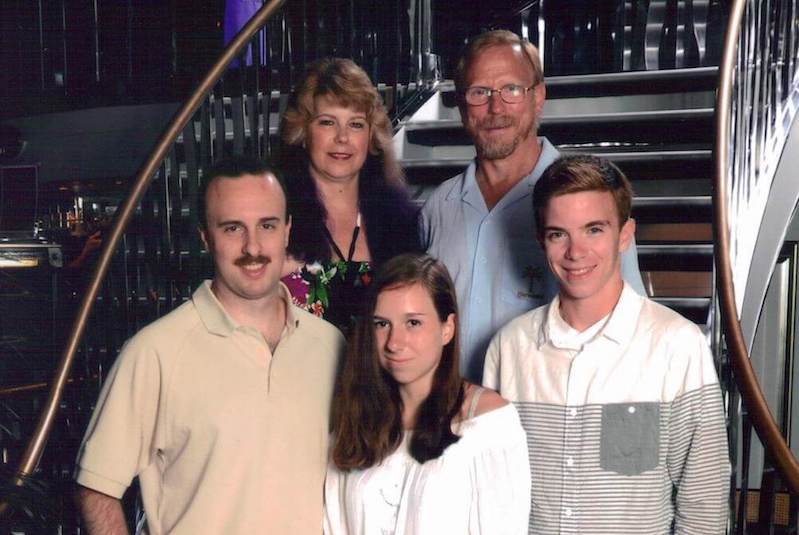
Felicia Walbridge has long been interested in biomedical engineering and plans on majoring in the field during college. Until recently, the teenager’s experience in this area was limited primarily to reruns of the TV show “Grey’s Anatomy.”
Then, with little warning, Walbridge became the star of her very own medical drama — complete with a hard-to-pronounce genetic mutation and a supporting cast of doctors and scientists from the Endocrine-Oncology Program at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center.
It started when the New Hampshire resident, then 14, had her wisdom teeth removed in 2016. An infection developed in her jaw, and when her oral surgeon could not pinpoint the cause, she was referred to Boston Children’s Hospital. Dr. Cory Resnick, an oral surgeon at Boston Children’s, ordered a biopsy that confirmed a bone infection. It also detected a suspicious mass in her neck.
“They had us get an MRI, and it turns out Felicia had a paraganglioma, a rare, slow-growing, tumor,” recalls Marguerite, Felicia’s mom. “So that was a very serendipitous infection; if she didn’t have it checked out, who knows how long we could have gone without finding the bigger problem?”
Diagnosis: Familial paraganglioma-pheochromocytoma syndrome
The tumor was removed in August 2017 by Dr. Reza Rahbar, an otolaryngologist/head and neck surgeon at Boston Children’s, and Felicia missed only the first week of her sophomore year of high school. After meeting with Jaclyn Schienda, a genetic counselor from the Endocrine-Oncology Program, Felicia and her family learned the cause of her tumor: a mutation in a gene leading to a genetic condition known as familial paraganglioma-pheochromocytoma syndrome.
It was a rare condition, but familiar to Felicia’s medical team, including oncologist Dr. Junne Kamihara, endocrinologist Dr. Ari Wassner, and surgeon Dr. Brent Weil. The Endocrine-Oncology Program at Dana-Farber/Boston Children’s brings together these and other experts in endocrinology, oncology, surgery, and cancer genetics to provide coordinated care to patients diagnosed with endocrine tumors.

“My doctors explained everything to me, and I had total confidence in them,” says Felicia. “I had to do eight months of antibiotics for the bone infection and start getting regular scans with Dr. Kamihara the next February, but everything seemed fine.”
Then came the next act of her drama.
An unexpected tumor
At her first follow-up scan, another mass was spotted in Felicia’s pancreas/abdominal area. It was a pseudopapillary tumor growing out of her pancreas; if left alone, it could become cancerous. By this point Felicia had become close to Drs. Kamihara and Weil, and was buoyed from her conversations with them.
“There was never any concern, because I knew my doctors could fix me,” says Felicia. “I needed more surgery, but they said I could wait until May, after I finished my AP (advanced placement) classes and exams.”
This operation at Dana-Farber/Boston Children’s, performed by Dr. Weil, kept Felicia in the hospital for a week. Then it was time for more watching and waiting.
“The pancreatic tumor was an unexpected finding, likely unrelated to the mutation she was found to carry. She took in the news with such maturity,” says Dr. Kamihara. “Felicia knows how excited we are that she hopes to become a biomedical engineer, and I know that she will use the experiences she has been through to help many other patients in the future.”
Moving forward since surgery
Since the operation, things have gone smoothly. Felicia’s most recent scan (in February 2019) was clean, with no signs of new tumors. Now a rising senior in high school, she is starting to look at colleges. Her parents hope she will stay close to home; this is fine with Felicia, because several schools in the Boston area have strong biomedical engineering programs. Her own experience has only heightened her interest in the field, even if it was not quite like “Grey’s Anatomy.”
“It’s been cool to learn about how my mutation works, but there wasn’t as much drama — and I didn’t get to watch my own surgery,” she says with a laugh.
Learn more about the Endocrine-Oncology Program at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center.
Related Posts :
-

‘Empowered to be there for Teagan’: New parents learn about hearing loss
Teagan O’Brien is a bright, spunky 4-year-old who loves reading, dancing, and playing outdoors. Her parents, Kim and Donnie, ...
-

A journey through the intestine during colitis, cell by cell
Inflammatory bowel disease (IBD), causing devastating abdominal pain, persistent diarrhea, and rectal bleeding, is hard to control with current treatments. ...
-

BRD7 research points to alternative insulin signaling pathway
Bromodomain-containing protein 7 (BRD7) was initially identified as a tumor suppressor, but further research has shown it has a broader role ...
-

Genetic variants are found in two types of strabismus, sparking hope for future treatment
Determining how genetics contribute to common forms of strabismus has been a challenge for researchers. Small discoveries are ...