Surviving stem cell transplant: New hope when the donor isn’t a full match
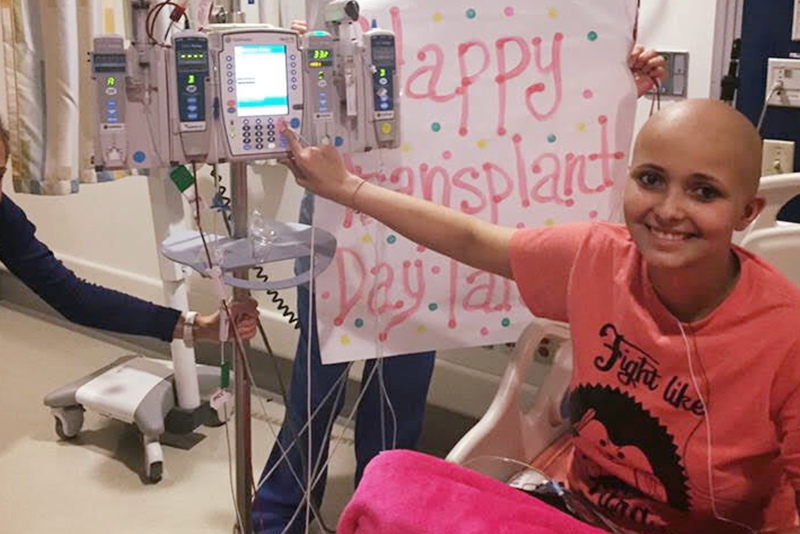
To see Tara Daniels today, with a corporate job in marketing and about to close on a house, you’d never know what she’s been through, how thrilled she is to be alive. This month marks five years since she received a high-risk bone marrow transplant for a life-threatening blood cancer.
Tara woke up feeling sick one morning in 2009, during her junior year of high school, and threw up. She powered through her midterm exams, but in the afternoon, she went to the doctor. She’d been having bad headaches and trouble breathing.
“The results of my blood tests came back, and they told my mom my immune system wasn’t working right,” she says. “I was rushed to Boston Children’s Hospital and didn’t leave for a month.” Oncologists at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center diagnosed Tara with acute lymphoblastic leukemia (ALL) and put her on a two-year chemotherapy protocol.

Tara, now 29, finished her treatment during freshman year of college. For most people with ALL, that would be the end of the story. But in her junior year, Tara relapsed and started a second course of chemotherapy.
“I did a semester of college from the hospital,” she recalls. “The school worked with me throughout to make sure I could graduate.”
But a year after graduation, Tara relapsed again. “My oncology team told me that this time, I had to get a bone marrow transplant,” she says.
A risky transplant
To have what’s now called a stem cell transplant, Tara first needed to find a donor with a matching tissue type — ideally matching on at least eight immune factors known as human leukocyte antigens (HLAs). Because her half siblings and parents weren’t a close enough HLA match, she found an unrelated donor through the Be The Match registry. However, transplants from unrelated donors pose a risk for graft-versus-host disease (GVHD), a life-threatening complication in which the donor’s cells attack the recipient’s own cells and tissues.
Tara’s oncology and transplant team, led by Dr. Jonathan Marron and Dr. Steve Margossian, made her an offer. A clinical trial called ABA2, led nationally by Dr. Leslie S. Kean and at Dana-Farber/Boston Children’s by Dr. Christine Duncan, was testing a treatment that might prevent GVHD. The treatment, abatacept, was an existing drug already being used for rheumatoid arthritis. Did she want to enroll?

There was just a 50:50 chance that Tara would receive abatacept, and a possibility that it wouldn’t work. But Tara said yes. She’d come this far and wanted to do whatever it took to make the transplant work, even if it meant rolling the dice.
Leveling the playing field
That was in 2016. This week, based on the results of ABA2, abatacept was officially approved by the U.S. Food and Drug Administration as the first-ever drug for GVHD prevention. Now available at Dana-Farber/Boston Children’s for eligible patients over age 2 who are receiving stem cell transplants from unrelated donors, abatacept will make stem cell transplant an option for many more children and adults with cancer and blood disorders.
Such transplants have historically been associated with an exceptionally high risk of severe, acute GVHD. But among those who received abatacept, survival rates were high. Only 2 percent developed severe GVHD in the first 100 days, versus 30 percent of controls who received standard transplant care.
“I see this as leveling the playing field for successful transplant for all ethnic groups,” says Dr. Kean, who directs the Stem Cell Transplant Program at Dana-Farber/Boston Children’s. “If you aren’t of Caucasian descent, you have way less than a 50 percent chance of finding an 8 of 8 HLA donor match, which is much less risky than a 7 of 8 match. But almost everyone has an 80 to 90 percent chance of finding a 7 of 8 match, and when you add abatacept, a substantially greater proportion can be transplanted safely.”
Likelihood of finding a matched donor, based on number of matching HLA factors
Many more people, especially those in non-white ethic groups, can find a bone marrow donor if they only need to match on 7 of 8 HLA factors. (Image adapted from: N Engl J Med 2014; 371:339-48.)
A chance at life
To this day, Tara doesn’t know whether she received abatacept or not. That’s typical of controlled clinical trials, where even the doctors are “blind” to the assigned treatment so as not to bias the results. But today, she’s back living her life, with her boyfriend, dogs, and plant collection, finally free of the “part-time job” of being a cancer patient. And she’s passionate about making treatments available to help others survive cancer.

“I will always advocate for research — we’re bettering the treatments, we’re bettering people’s chances,” Tara says. “If research hadn’t been done on transplants over the years, I wouldn’t be alive today.”
Learn more about the Hematopoietic Stem Cell Transplant Program at Dana-Farber/Boston Children’s.
Related Posts :
-

Arthritis drug reduces rates of acute graft-vs-host disease after bone marrow transplant
The immune-suppressing drug abatacept, currently used for rheumatoid arthritis, could make bone marrow transplant safer, report researchers at the Dana-Farber/...
-

Looking for clues to improve the life of a transplanted organ
The Transplant Research Program (TxRP) at Boston Children’s Hospital is the only pediatric transplantation research program in the U....
-

Stem cell transplant leads Ali to remission, and a new home
The journey that led Ali Mercy to Dana-Farber/Boston Children’s began in 2010, when Ali was diagnosed with acute lymphocytic ...
-

Poverty predicts worse cancer outcomes, even in children receiving top-tier care
A pair of recent studies suggests that even among patients receiving advanced cancer care, poverty is a predictor of worse ...