Vacuum bell therapy: A nonsurgical option for chest wall depression (pectus excavatum)
Pectus excavatum is one of the most common chest wall abnormalities, affecting about 1 in 300 children. Physicians at Boston Children’s Hospital helped define early treatments for chest wall problems and continue to develop innovative approaches to pectus excavatum. These innovations include a nonsurgical procedure called vacuum bell therapy. While children with severe pectus excavatum often need surgery, vacuum bell therapy may make surgery unnecessary.
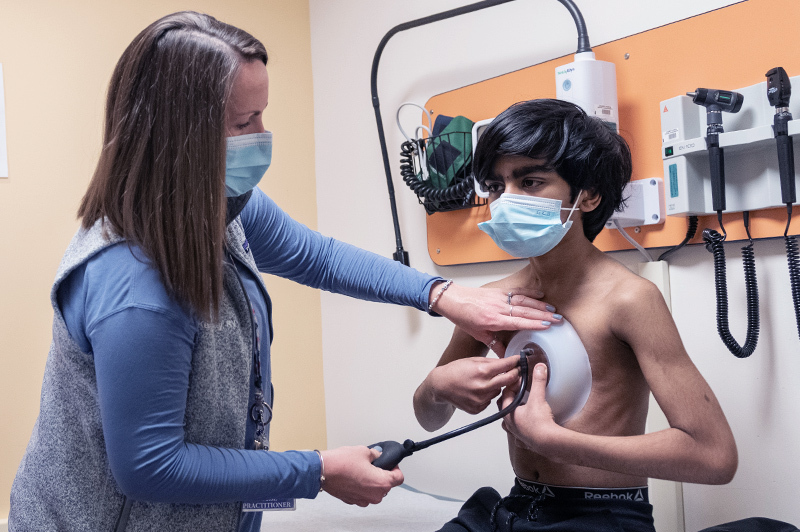
Here, Kelly Bartkus, a nurse practitioner in the Pectus and Chest Wall Treatment Program who has cared for many patients with pectus excavatum, answers questions about the vacuum bell procedure and offers advice to help kids.
How does vacuum bell therapy work?
Pectus excavatum is a chest wall abnormality that causes a depression in the middle of the chest. This can develop at birth or develop when your child is older. This condition is often apparent during adolescence and can become more severe during growth spurts.
The vacuum bell is a cup-shaped device made of soft rubber that’s connected to a hand pump. The device is placed on the child’s chest and the pump is used to create suction. This suction slowly pulls the breastbone forward. After a period of consistent use, the breastbone and ribs stay forward on their own. Many patients notice improvement in their chest wall depression in the first three to four months.
How much time do patients have to spend wearing the device a day?
The goal is to wear the device for two hours, twice a day, but patients work their way up to this. At first, patients typically wear the device for about 30 minutes twice a day, then add 15 minutes each week. It should take about six weeks to reach a wear time of two hours twice a day.
Is vacuum bell therapy painful?
Vacuum bell therapy is not painful. Patients say they feel pressure when the device is first applied. But the treatment should not cause pain or feel uncomfortable. We tell families to contact us right away if it does.
Can kids go to school wearing the vacuum bell?
The device can be worn during regular activities throughout the day, however, we recommend wearing the device before or after school so that kids don’t have to put it on or take it off during school hours.

What activities should a child avoid while wearing the vacuum bell?
We recommend not wearing the device during gym class or contact sports. Likewise, the vacuum bell should not be worn while swimming or playing in the water. If a patient wants to apply the vacuum bell directly after these activities, it’s important to make sure their skin is completely dry.
What if my child feels self-conscious wearing the device?
If your child is self-conscious about how they look wearing the device, we recommend they only wear it at home. The vacuum bell is worn on a bare chest but kids usually wear a t-shirt or sweatshirt over it to cover the device. Depending on the clothing and material, the device may not be noticeable to others.
How long does vacuum bell treatment last?
Most kids use the device for at least one year. The length of treatment varies depending on the patient’s age, how old they were when they started vacuum bell treatment, and how severely their chest sinks inward.
Should parents or patients be concerned about side effects from the vacuum bell?
Some patients who undergo vacuum bell therapy report mild side effects, such as bruising, sore chest and back muscles, redness or skin irritation, and flabby skin. These side effects are usually temporary. If they do occur, we recommend wearing the device for shorter periods of time or reducing the pressure of the device (controlled by the number of “pumps”) until they subside.
What can families do to increase their chance of success with vacuum bell therapy?
Vacuum bell therapy is more effective when it begins when a child is about 11 years old. Children who start out with a mild chest wall depression and who use the device consistently have the greatest chance that the therapy will be successful.
Learn more about the Pectus and Chest Wall Treatment Program.
Related Posts :
-

“Observe. Be open.”: How Boston Children’s nurses are changing the future of global health
Ashley Birch, MSN, CPNP, a Boston Children’s pediatric nurse practitioner and Global Nursing fellow, didn’t expect a trash ...
-

Nurse-led innovations: A virtual-nursing pilot helps nurses thrive
It was night shift on the 9E Inpatient Medical Unit and Marisol Hernandez, BSN, RN, CPN, was helping another nurse ...
-

In a thriving gene therapy program, nursing leadership is the driving force
Gene therapy was made possible by decades of technological advances. But to execute gene therapy at scale? That would not ...
-

‘The reason I became a nurse’: Maeve’s memories of laryngeal cleft repair
Being a gastroenterology nurse is more than a profession for Maeve Lee. When she cares for patients with feeding tubes, ...





