GALLERY: Custom-built ‘trainers’ help clinicians master procedures

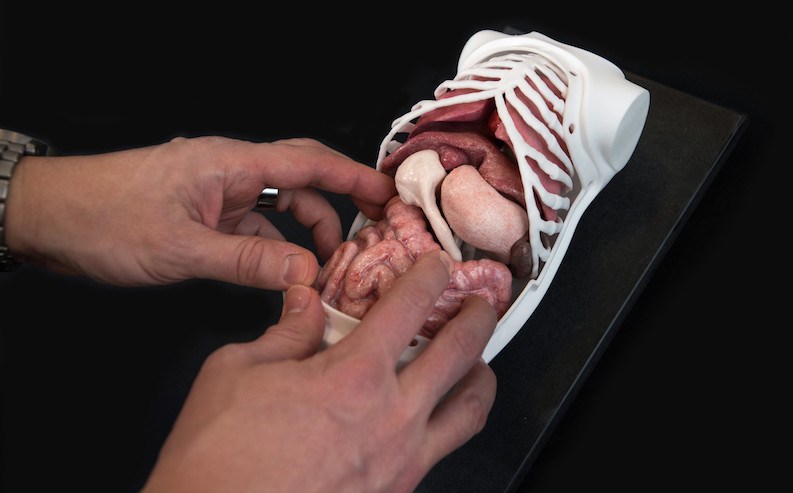
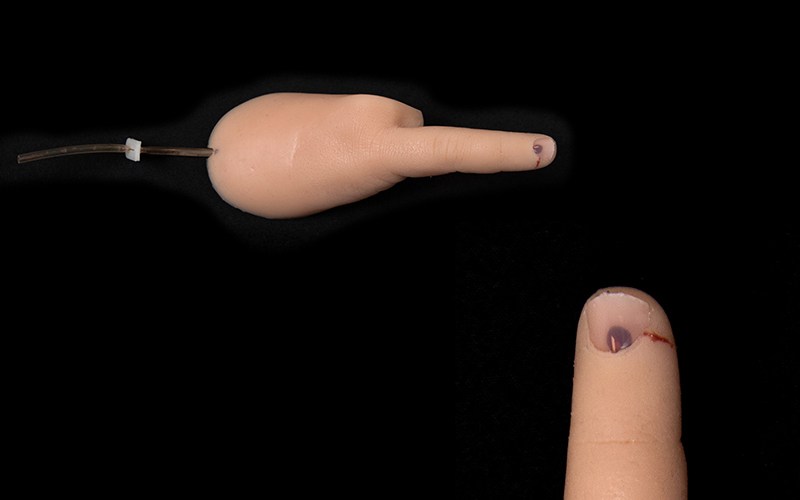
Walking into the SIMPeds Engineering Studio, a few blocks from Boston Children’s Hospital, the first thing you notice is body parts — high-fidelity replicas of human anatomy in various sizes. Some are in a glass display case, while others are laid out in various states of assembly, from a lone finger to the complete abdominal cavity of a newborn, packed with diminutive organs. Six newborn-sized, hollow duodenums, cast in rubber over a plastic mold, hang ready near a workbench.
These aren’t your usual medical mannequins.
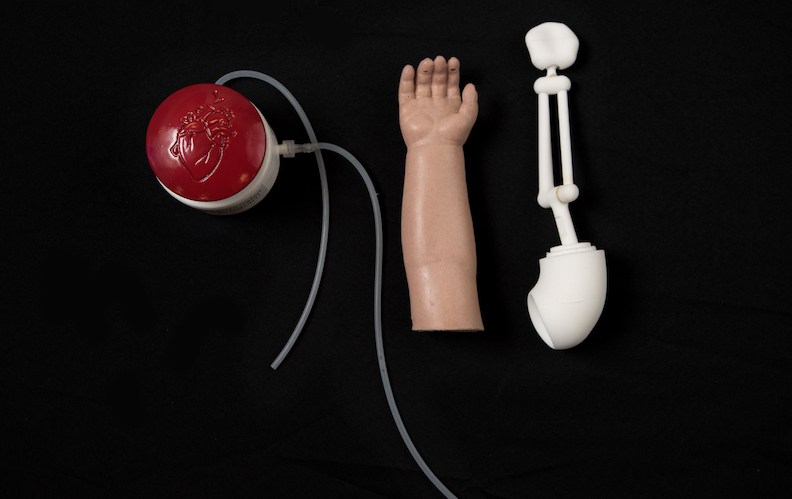
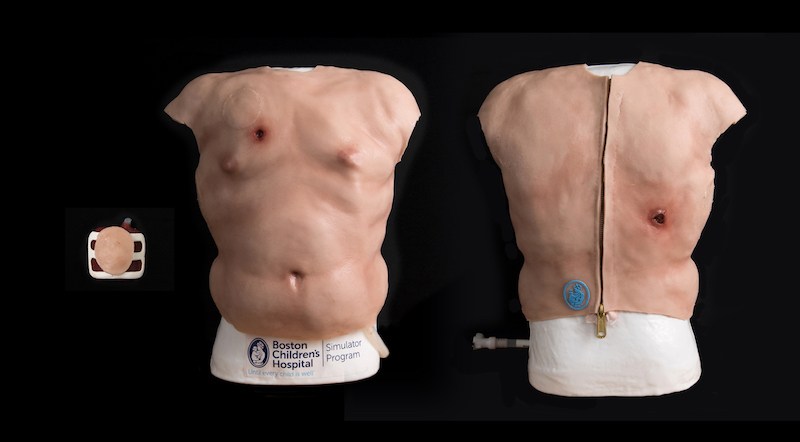
In the adjoining InventorSpace, three 3D used by surgeons to rehearse an upcoming complex operation. Others are used for general training and preparedness purposes. A collaboration with the special effects company Fractured FX helped launch the first trainers; today there are more than 20 in various stages of development. They allow practice of rare or infrequently performed procedures as well as some common ones that pose challenges in children.
Knowing the nose

Not your average doll arm
Zip-on trauma practice
Addressing atresia
Taking the trepidation out of trephination
The thigh bone’s connected

Cath port confidence

Fabrication at their fingertips

Each trainer represents a close collaboration between clinicians and SIMPeds simulation engineers Greg Loan, Andrew Hosmer, Katie Livingston, Noah Schulz, Mariah Geritano, Duncan Smith-Freedman and Reimi Yonekura. Maeve Geary, a PhD candidate from Bolton University (U.K.), also contributes to the designs.
Plenty of new trainers are on the drawing board or in the early stages of construction. While priority for custom trainers is given to clinicians at Boston Children’s, outside requests will be entertained. “We have seven engineers and a large capacity for fabrication,” says Melissa Burke, director of Business Development for Boston Children’s Simulator Program.
Learn more about SIMPeds and SIMEngineering
Related Posts :
-

AI-enabled medical devices are burgeoning, but many haven’t been tested in children
Medical devices that incorporate artificial intelligence and machine learning are proliferating. In 2013, the FDA approved fewer than 10 such devices; by 2023, ...
-

‘Zero place for mistakes’: Taking fetal surgery to the next level with simulation
The highly complex interventions involved in fetal surgery require exceptional skill, training, and experience. Beyond the procedures themselves, these surgical ...
-

Simulation-based training program improves evaluation of undescended testicles
Could a lifelike manikin torso help improve pediatricians’ understanding of undescended testicles? That’s the hope of Eric Bortnick, MD, ...
-

The people and advancements behind 75 years of Boston Children’s Cardiology
Boston Children’s Department of Cardiology has more than 100 pediatric and adult cardiologists, over 40 clinical fellows learning the ...





