Chasing Rett syndrome biomarkers: Could overnight EEG studies improve care?
In Rett syndrome, a genetic condition affecting girls almost exclusively, mutations in the MECP2 gene cause a regression of language and motor skills starting at 12 to 18 months of age. Children then usually stabilize, but how Rett will ultimately affect them is hard to predict. Some girls develop epilepsy; others have no seizures at all. Language, cognitive, and fine motor function varies widely.
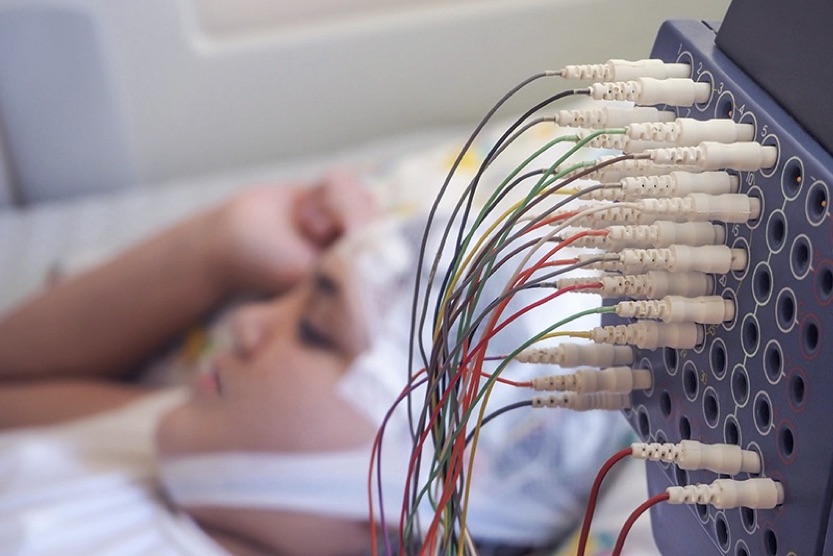
Preliminary research led by Patrick Davis, MD, PhD, a resident in the Department of Neurology at Boston Children’s, and April Levin MD, a faculty researcher and neurologist, suggests that overnight EEG studies could someday help clinicians and families know what to expect and help inform care for girls with Rett syndrome.
“There is a huge range of symptom severity in Rett syndrome,” says Davis. “For example, language development can range from relatively normal, to being able to have simple conversations, to having no words and no language comprehension. We currently have no reliable way to predict, much less modify, this developmental trajectory. A biomarker would be a step toward developing more refined interventions.”
The rhythms of the night
EEG studies in Rett syndrome aren’t new, but are almost always done while the child is awake. Davis, Levin, and and their colleagues, Kyle Takach and Kiran Maski, MD, MPH, wanted to see what happens to the EEG during sleep.
“Sleep is an active time when the brain processes new information and rewires to optimize its functioning,” says Davis. “We reasoned that altered brain activity in sleep might contribute to neurodevelopmental problems in Rett syndrome. There’s a rich literature on sleep EEGs, but few studies have looked at Rett syndrome specifically.”
The retrospective study analyzed overnight EEG data from 22 girls with Rett syndrome who had EEGs ordered by clinicians (most likely to evaluate seizures) and 25 age-matched, typically developing children who served as controls. The researchers tracked the different frequency waves that make up the EEG signal, each created by the collective firing of large groups of neurons.
Specifically, they focused phase-amplitude coupling — a measure of how slow EEG oscillations, which are important for memory consolidation — relate to higher-frequency waves. This relationship is thought to reflect how well brain activity is integrated.
And that is where children with Rett syndrome clearly diverged. Typically developing children showed a close coupling of slow and fast oscillations at the top of the brain, starting at around 12-to-18 months of age. The children with Rett syndrome never developed that feature. Instead, they developed clearly different patterns of couplings of slow and fast oscillations in various brain locations.
“Just by looking at the sleep EEG, we could predict whether a patient had Rett syndrome or not with 90 percent accuracy,” says Davis. “We also found specific EEG patterns that may correspond to different subtypes of Rett syndrome or even help predict clinical severity.”
Long-range goals: Rett syndrome and beyond
Davis emphasizes that this work is just a first pass in a small, select group of patients and needs to be confirmed and expanded upon. It also does not prove that the altered EEG patterns are the cause of neurodevelopmental regression in Rett syndrome. But Davis is excited about the possibilities the work brings up.
“If we can validate our findings in a larger cohort of girls with Rett, it would be interesting to see if doing noninvasive brain stimulation at night — with a cap worn during sleep — could improve some EEG biomarkers, and whether targeted brain stimulation would improve a child’s developmental trajectory,” he says. “That is one of our ultimate goals.”
Transcranial magnetic stimulation is already being tested in children with epilepsy and has been proven safe. It could provide an alternative to epilepsy or sleep medications, which come with many side effects, or it could be used in combination with drugs. Further EEG studies in girls with Rett syndrome could point the way to particular brain circuits to target with brain stimulation.
Davis and his colleagues are also interested in looking at overnight EEGs in children with Rett syndrome who don’t have epilepsy, and in children with other early-onset disorders that involve altered sleep dynamics, such as epileptic encephalopathies, infantile spasms, trisomy 21, and autism spectrum disorder.
“The development of reliable biomarkers is a key step toward identifying the best anti-seizure medications and developing pharmacologic treatments for the cognitive and intellectual symptoms for these disorders,” Davis says. “We think overnight EEGs could be the foundation of meaningful translational work.”
Learn more about Boston Children’s research on Rett syndrome.
Related Posts :
-

“Princess June” reigns supreme over Rasmussen syndrome
What do you call a “girly” 5-year-old who adores dolls and frilly nightgowns? If you’re one of June Pelletier’...
-

The thalamus: A potential therapeutic target for neurodevelopmental disorders
Years ago, as a neurology resident, Chinfei Chen, MD, PhD, cared for a 20-year-old woman who had experienced a very ...
-

Could peripheral neuropathy be stopped before it starts?
An increase in high-fat, high-fructose foods in people’s diets has contributed to a dramatic increase in type 2 diabetes. This, ...
-

Status epilepticus: What’s changed, what to know, and a global perspective
Status epilepticus, or a prolonged seizure lasting more than five minutes, is a rare complication of epilepsy and a medical ...





