Is rapamycin the new aspirin?
I’ve heard it said that if aspirin had to go through today’s FDA approval process, it would never be approved for over-the-counter use because it just does so many things. Lately, it’s been hard to cover biomedical research at Children’s without stumbling on another drug that’s also FDA-approved and also seems to have multiple uses: rapamycin.
It’s a drug that targets a pathway fundamental to nearly every cell in the body, yet is seemingly good for nearly everything. But how can one drug touch on so many cells and tissues and organs and still be both effective and safe?
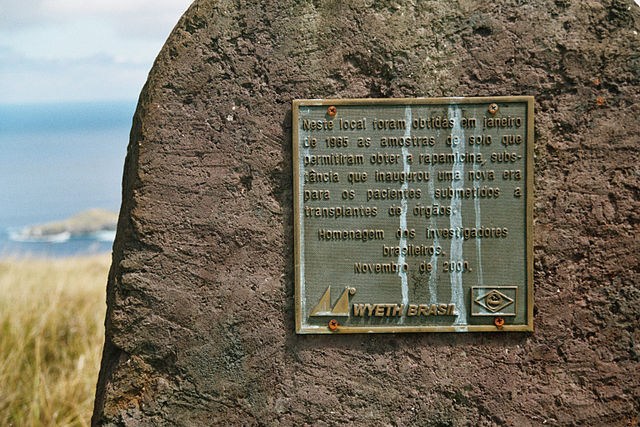
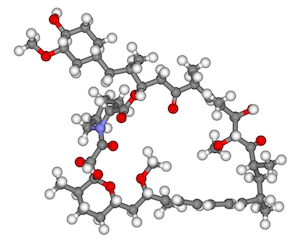
First found in the 1960s in soil bacteria collected on Easter Island (the drug’s name comes from the island’s native name, Rapa Nui), rapamycin is a naturally derived antibiotic, antifungal and immunosuppressant. It is commonly used to prevent rejection in organ or bone-marrow transplant patients. It also holds the distinction of having been one of the first drugs to have its target identified biochemically: the aptly named protein “mammalian target of rapamycin,” or mTOR.

Since its discovery, researchers have found that mTOR plays a central role in the life of the cell: It acts as kind of a cellular router, directing signals from outside the cell to mechanisms that drive processes related to cell growth, protein production and metabolism. It also influences the growth of blood vessels, or angiogenesis, and has a role to play in helping stem cells retain their “stem-ness” – two important functions that influence the growth of tumors.
While growth and metabolism are sort of a common thread, what has struck me is the broad range of diseases in which rapamycin and its descendants are being studied as possible treatments, from vascular malformations to neurocognitive disorders, premature aging disorders to kidney disease, genetic cardiomyopathies to multiple kinds of cancer.
“The mTOR pathway is involved in so many cellular processes, which is why it is found to be involved in so many different settings,” says Joyce Bischoff, a vascular biologist studying mTOR in the context of hemagiomas, a group of vascular anomalies characterized by overgrowth of masses of blood vessels. “It is also highly regulated, so there are many opportunities for it to become dysregulated.”
Apart from its preference for a ubiquitous target, rapamycin has long list of attractions as a potential therapy in pediatrics, at the top of which is its longevity: It’s been used for nearly two decades. “There is a long history of using rapamycin in children. We know what the side effects are, and they are relatively mild,” points out Amy Roberts, a cardiovascular geneticist who is putting together a trial of rapamycin for cardiomyopathies caused by mutations in genes that affect mTOR. “The fact that it’s already FDA approved, well understood biochemically, and has an good safety profile means that it is relatively easy to bring it into the clinic for other conditions.”
“One thing we know about the mTOR pathway is that you need the right amount of signaling in order to avoid disease.”
In citing rapamycin’s safety profile, Roberts raises an interesting point: If mTOR is the junction box for so many fundamental functions in so many cells and tissues, why is rapamycin not wildly toxic? One answer could be that like most inhibitory drugs, rapamycin isn’t 100 percent effective. Rather, it allows some signaling to leak through, suggesting that its real mechanism of action in all of these diseases is to bring uncontrolled signaling to a more healthy level. “One thing we know about the mTOR pathway is that you need the right amount of signaling in order to avoid disease,” says Bischoff. “It’s when cells have too much or too little mTOR activity that you see problems.”
Scott Armstrong – a hematologist with Dana-Farber/Children’s Hospital Cancer Center (DF/CHCC) who, along with Lewis Silverman, is running a trial aimed at blocking mTOR in pediatric leukemias – offers a second theory, one that also touches on mTOR’s different roles and effects in different tissues: “What a cell is and does is determined by which of its genes are turned on and off. mTOR is going to have different effects in blood cells and heart cells and neurons because while it helps all of these cells process signals from outside, how those signals are perceived by the cells depends on the genes that are available to ‘hear’ the signal.”
Rapamycin will come off patent in a couple of years, opening up the market for generic production and potentially lowering the drug’s cost. And its story doesn’t end there: Companies like Pfizer and Novartis are working on next generation mTOR blockers like RAD001 (a Novartis drug) that promise greater specificity and efficacy. “There are a lot of mTOR inhibitors in the pipeline,” according to neurologist Mustafa Sahin, who thinks this rapamycin descendent could help children with tuberous sclerosis, a neurocognitive condition caused by miswiring within the brain. “And with the growing interest in rare diseases, I’m pretty confident companies will continue to put resources toward this pathway.”
Related Posts :
-

The dopamine reset: Restoring what’s missing in AADC deficiency
In March 2023, a young girl came to Boston Children’s Hospital unable to hold up her head — one striking symptom ...
-

Parsing the promise of inosine for neurogenic bladder
Spinal cord damage — whether from traumatic injury or conditions such as spina bifida — can have a profound impact on bladder ...
-

Unveiling the hidden impact of moyamoya disease: Brain injury without symptoms
Moyamoya disease — a rare, progressive condition that narrows the brain’s blood vessels — leads to an increased risk of stroke ...
-

A new druggable cancer target: RNA-binding proteins on the cell surface
In 2021, research led by Ryan Flynn, MD, PhD, and his mentor, Nobel laureate Carolyn Bertozzi, PhD, opened a new chapter ...