Pharmacogenomics: Nearly 30 percent of children could benefit, study finds
Medications aren’t one-size-fits-all. Genetic differences can affect how patients metabolize drugs, and can sometimes make a beneficial drug ineffective or even toxic. In one infamous case, a 2-year-old boy in Canada died from a codeine dose he received after surgery. A genetic difference caused him to metabolize codeine so quickly that toxic levels of morphine (a codeine break-down product) built up in his blood.
Situations like this led Boston Children’s Hospital to establish the Clinical Pharmacogenomics Service. Founded in 2011 by Shannon Manzi, PharmD, together with the Division of Genetics and Genomics, it is one of a handful of such centers in the country. Care providers within or outside Boston Children’s can request a pharmacogenomic analysis before prescribing if they are concerned about possible side effects, drug reactions, or lack of response to a medication. Families can also initiate the request, but will require a referral for insurance purposes.
Testing includes analysis of genes affecting medication breakdown, transport, and response. A study published Jan. 8 in the journal Genetics in Medicine shows that tapping into patients’ genomes could greatly improve prescribing — even for everyday conditions.
Improving drug safety with genomics
Manzi teamed up with Dianbo Liu, PhD, Karen Olson, PhD, and Kenneth Mandl, MD, MPH, in the Computational Health Informatics Program (CHIP) at Boston Children’s. Together, they analyzed pharmacy claims from more than 2 million people nationwide, including more than 400,000 children.
“As our understanding of the impact of pharmacogenomics on safe medication use has grown, we wanted to understand how many patients this knowledge could benefit,” says Manzi. “With the expertise of CHIP and this large claims database, we could begin to answer this question.”
Our study points to opportunities to include reminders in electronic health records, so that prescribers can take genomics into account in real time.” — Kenneth Mandl
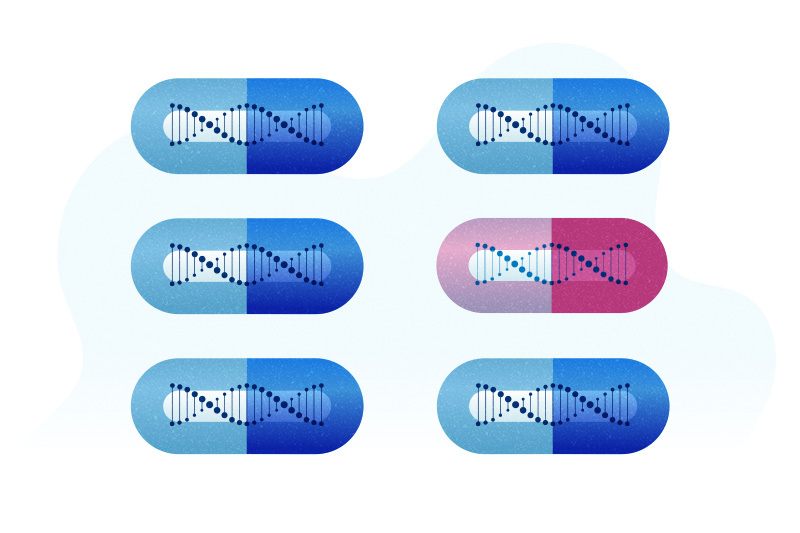
A surprising 63 percent of adults and 29 percent of children were prescribed medications whose effects could differ based on their genetics. Ten percent of people studied were prescribed more than one such medication at a time for at least 30 days. Many of the medications were extremely common, like ibuprofen and codeine.
Knowing a patient’s genetics could prompt a medical provider to choose a different drug, change the dosing regimen, or provide closer monitoring to make sure the drug is working and not causing harm, says Manzi.
A pharmacogenomics future?
Right now, very few medical practices have a system for routine genetic screening before prescribing medications. But this study shows there’s lots of opportunity for pharmacogenomics to improve care. Researchers have identified hundreds of genes affecting medication metabolism, some of them currently listed on medication labels.
“Our study points to opportunities to include reminders in electronic health records, so that prescribers can take genomics into account in real time,” says Mandl. “With technologies that CHIP has developed, this could be adopted at national scale.”
Learn more about the Pharmacogenomics service at Boston Children’s Hospital
Related Posts :
-

Pharmacogenomics: One size doesn’t fit all
In 2009, The New England Journal of Medicine reported the case of an otherwise healthy 2-year-old boy in Canada ...
-

Making genome sequencing a first-line test in rare disease
Children with rare diseases often undergo years of medical visits and genetic testing before they get a diagnosis. Over the ...
-

The gut-brain connection: A new approach to OCD and tic disorders?
It’s natural for young children to use routines to help them navigate the world and for older children and ...
-

Two rising stars in kidney genetics: Nina Mann and Amar Majmundar
A healthy, functional kidney must maintain a delicate balance of water, nutrients, and electrolytes so it can properly filter the ...