A unique marker for pericytes could help forge a new path for pulmonary hypertension care
Pulmonary arterial hypertension (PAH) is a rare condition that’s difficult to treat. The hallmarks of the disease — narrowing of the arterioles and capillaries that deliver blood to the lungs — force the heart to work harder. In severe cases, PAH can lead to heart failure.
Pericytes support capillary function and may play a role in PAH, but because they’re so difficult to study, few researchers have pursued this question.
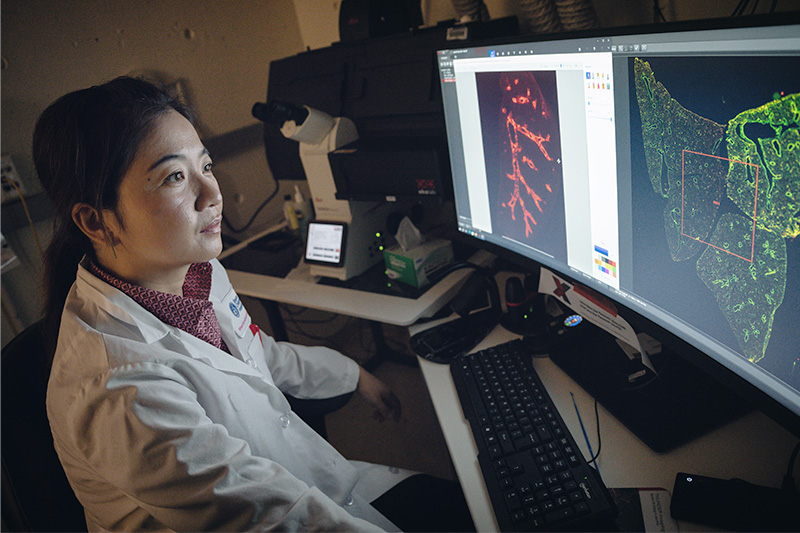
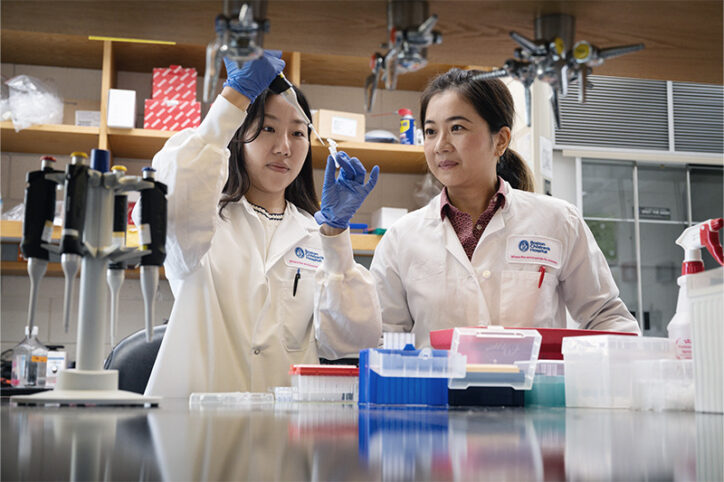
Tiny and chameleon-like, pericytes share markers with several other pulmonary cells, including smooth muscle cells, fibroblasts, and myofibroblasts. Ke Yuan, PhD, an associate scientific researcher in Boston Children’s Division of Pulmonary Medicine, has long suspected pericytes contribute to PAH. But without a way to identify them in a sea of other cells, studying pericytes’ role in pulmonary disease has been challenging.
This pursuit recently became more promising. For the first time, the Ke Yuan Lab has identified a pericyte-specific marker with implications that could change the course of PAH research and treatment.
When cells change teams
For years, researchers have studied the role of vascular remodeling in the development of PAH. Triggered by hypoxia — a deprivation of oxygen, such as with certain congenital heart defects or lung disease — endothelial cells change the shape and function of smooth muscle cells. In essence, when deprived of oxygen, endothelial cells abandon their supportive role along the lining of capillary walls and obstruct the blood vessels instead.
This was part of the puzzle. But what about pericytes? Do they too undergo vascular remodeling and contribute to PAH?
In search of a pericyte marker
In a previous study, the Yuan lab found that pericytes seem to transform into smooth muscle cells with the help of hypoxia-inducible factor 2a (HIF2a) — a gene that helps the body adapt to changing oxygen levels. They also found that high levels of HIF2a exacerbate pulmonary hypertension and right ventricular hypertrophy in transgenic mice. The team published their findings in EMBO reports.
Encouraged by these results, they wanted to study how pericytes change their lineage to contribute to PAH. Such information, they believed, could be used to design therapies to prevent the transformation. But to gather it, they needed a way to identify the elusive cells.
“A unique marker to label pericytes would enable us to exclusively study their role in pulmonary diseases,” says Yuan.
That unique marker came in the form of the gene Higd1b. Using it, the team was able to identify two types of pericytes that had two different reactions to hypoxia: Type 1 remained dormant; Type 2 contributed to pulmonary disease by moving into the arterioles and taking on the characteristics of smooth muscle cells. The follow-up study appeared in the EMBO Journal.
Obscure no more
Pericytes were first described in the 1870s. A century and a half later, researchers can now use Higd1b to study pericytes exclusively, apart from other cells. This could open new therapeutic pathways for PAH and several other pulmonary issues.
“We can use Higd1b as a tracing tool to study how pericytes change their cell fate and location under disease settings such as asthma, COPD, and pulmonary fibrosis,” says Yuan. “This could empower future investigations to delve into the dynamic role of pericytes in disease development and pave the way for disease-modifying therapies.”
While Yuan’s lab is focused on the role of pericytes in pulmonary disease, their discovery of a specific marker could help accelerate treatments for other diseases as well. Given how pervasive pericytes are throughout the body, this breakthrough could spur new approaches to treating diabetic retinopathy, heart disease, Alzheimer’s disease, and many other conditions.
Refer a patient to the Pulmonary Hypertension Program.
Related Posts :
-

Study suggests hypoxia overexpression causes pericytes to contribute to pulmonary hypertension
Pericytes, the multifunctional cells that work within the walls of capillaries, have been a subject of focus in the study ...
-

The ‘Trach Chapter’: Isabella’s journey with bronchopulmonary dysplasia
Isabella’s life has been anything but ordinary. Born at just 27 weeks gestation and weighing only 1 pound, 4 ounces, Isabella has ...
-

Promising advances in fetal therapy for vein of Galen malformation
In 2024, Megan Ingram* of California and her husband were preparing for the birth of their third child when a 34-week ...
-

Four things you should know about MAPCAs treatment
As the first grandchild in her family, Hannah Homan is in demand for frequent visits. She was also the focus ...