DIY pain relief with light-activated local nerve blocks
You’ve just had a root canal or knee surgery — both situations that will likely require some sort of local pain medication. But instead of taking a systemic narcotic with all its side effects, what if you could medicate only the part of your body that hurts, only when needed and only as much as necessary?
That concept is today’s reality in the laboratory of Daniel Kohane, MD, PhD, professor of anesthesia at Harvard Medical School and a senior associate in pediatric critical care at Boston Children’s Hospital.
The Kohane laboratory is developing a patient-triggered drug delivery system — but not a simple time-release mechanism or one tethered to ports or pumps. Instead, around the time of an intervention, pain medication would be injected into the site, or around a nerve leading to that site. Whenever pain relief is needed, the patient triggers release of the drug with a laser-like light-emitting device. “It’s like carrying the pharmacy in your body,” explains Kohane.
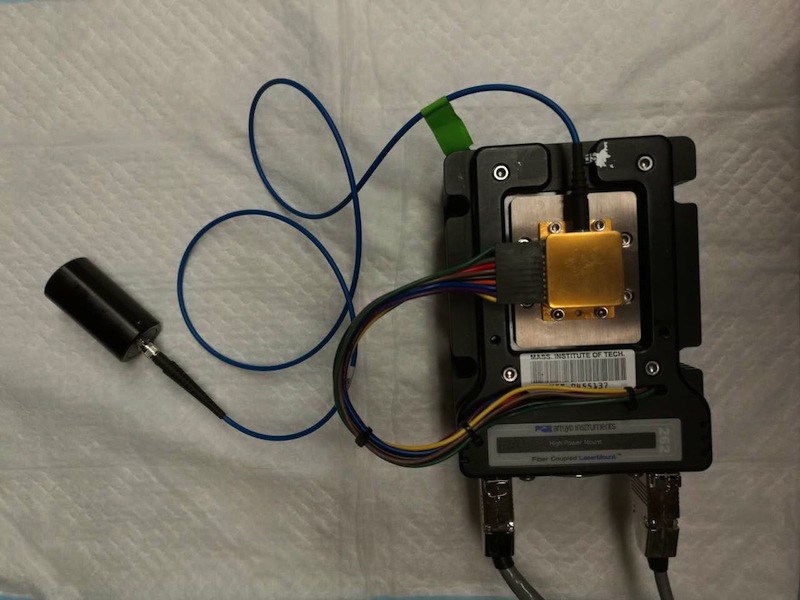
Kohane developed the concept with graduate student Alina Rwei and postdoc Changyou Zhan. The analgesic is packaged inside liposomes — particles made out of lipid shells — that are coated with gold nanoparticles. When irradiated by near infrared (NIR) light, the gold particles heat up, in turn heating the fatty liposomes which become leaky and release their analgesic payload.
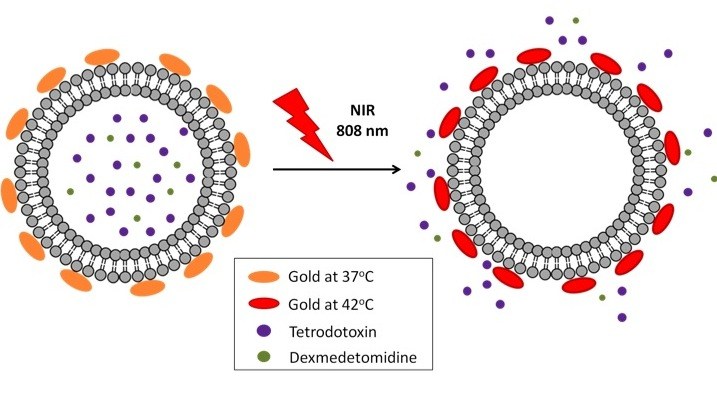
As Kohane described in a TEDMED talk, patients would apply NIR light directly at the site of the pain, releasing drug as often or as long as needed. (NIR light devices are already readily available and considered safe at low energy levels.) How much analgesic patients receive would depend on how strong the light is and how long they irradiate the area. “The patient could determine when they get pain relief, how intense the pain relief was and how long it lasted,” Kohane says.
Potent marine analgesics
The actual analgesics of interest to Kohane are neurotoxins derived from marine sources that block sodium channels conducting pain messages; examples include tetrodotoxin (TTX), saxitoxin and neosaxitoxin. Found in pufferfish, TTX can cause serious food poisoning when the fish is not prepared well, but in small quantities it has long been shown to be safe and powerful local anesthetic.
Coupled with these local nerve-blocking drugs, a NIRS-activated pain relief system also may allay the serious public health epidemic of narcotic overuse, addiction and overdose. “If we can get this to work well, and to work enough times to eliminate the pain safely, we can potentially provide on-demand, completely controllable pain relief without any systemic narcotics at all,” says Kohane.
The concept’s success has already been proven in animal tests. Within the last year, Kohane and colleagues have published several studies showing this triggerable TTX/NIR-induced system provided rat footpad analgesia and relief of pain in areas innervated by the sciatic nerve in rats.
Cancer and eye disease
Going forward, Kohane and colleagues are optimizing their concept with the goals of being able to penetrate deeper into tissue, to use less and less energy (which is also important for safety reasons) and to allow medication to be triggered many times. This may also mean using other triggering sources, like magnetic fields or ultrasound.
The Kohane laboratory and others are also looking to extend this form of drug delivery to relieve eye pain due to injury or after surgery and for cancer nanomedicine approaches to targeted cancer imaging and treatment. “We are working on several paths to the same thing,” Kohane says, “safe, effective drug delivery systems that work better than the ones we have now with little or no toxicity.”
Alice McCarthy is a science writer covering biomedical research and the latest in new medical treatments.
Related Posts :
-

A new druggable cancer target: RNA-binding proteins on the cell surface
In 2021, research led by Ryan Flynn, MD, PhD, and his mentor, Nobel laureate Carolyn Bertozzi, PhD, opened a new chapter ...
-

Modeling urinary tract disorders on a chip: Zohreh Izadifar
When a new tissue sample arrives from the Department of Urology, the Boston Children’s Hospital lab of Zohreh Izadifar, ...
-

Could a pill treat sickle cell disease?
The new gene therapies for sickle cell disease — including the gene-editing treatment Casgevy, based on research at Boston Children’s ...
-

Injected microbubbles could be a safe way to deliver emergency oxygen
For years, researchers and clinicians have been trying to find a way to rapidly deliver oxygen to patients when traditional ...