Low-carb diets for diabetes: Rediscovering centuries-old wisdom

This year represents the 100th anniversary of the discovery of insulin, a hormone that regulates the amount of glucose, or sugar, in the blood. While insulin medications have literally been life-savers for many kids and adults with diabetes, diets that help keep blood sugar levels steady are often overlooked for controlling diabetes. These diets, often referred to as low-carbohydrate diets, restrict the daily amount of carbohydrate-rich foods, like breads, pasta, and potatoes. Sometimes known as low-glycemic diets, they help prevent blood sugar levels from spiking or dropping too quickly, which can be dangerous for people with diabetes.
In a special issue of the Clinical Journal of Investigation commemorating insulin’s 100th anniversary, researchers from Boston Children’s Hospital summarized the history of low-carbohydrate diets and argued that they might help transform clinical care today.
Studies show low-carb diets help stabilize blood sugar
People with type 1 diabetes can’t make enough insulin naturally so they need to take insulin medications. Those with type 2 diabetes don’t require extra insulin.
When the researchers studied the history of low-carb diets in diabetes, they found scientific evidence that these diets are a good way of controlling blood sugar in people with type 2 diabetes. Several large clinical trials showed that diet alone can often eliminate the disease and allow people to stop taking medications.
“Despite vast amounts of money spent for insulin and other treatments, diabetes continues to lower life expectancy and quality of life severely,” says Dr. David Ludwig, of the Division of Endocrinology and co-director of the New Balance Foundation Obesity Prevention Center at Boston Children’s who led the study. “Low-carb diets, in addition to insulin use when needed, offer to transform this situation, promising an inexpensive treatment aimed at the cause of the problem: intolerance to carbohydrate in the diet.”
Diet was standard treatment before insulin
Eating a low-carbohydrate diet was the standard treatment for diabetes as far back as the 1700s before the discovery of insulin, capable of curing type 2 diabetes in adults or extending life, in some cases for years, in type 1 diabetes in children.
“After insulin came a huge sigh of relief,” says Dr. Belinda Lennerz, an endrocrinologist at Boston Children’s who also conducts diabetes research in the Ludwig laboratory. “The thinking went, we have a treatment for this and we don’t have to be on a low-carb diet anymore.”
But within 20 years, the pendulum swung so that high-carbohydrate diets became the norm — simply because insulin allowed people to eat carbohydrates without immediate complications.
In addition, modern technology such as continuous blood glucose monitoring, specialized versions of insulin, and other drugs for diabetes complications, has greatly improved the lives of people with diabetes.
Mismatch between carb intake and insulin peak
When we eat processed carbs, our blood sugar peaks in about 30 minutes. But insulin action doesn’t kick in until an hour and continues for a few hours. This is true for everyone, not just those with diabetes.
“One of the big challenges in diabetes care is this mismatch that you always have between carb intake and estimating how much insulin you’ll need,” explains Dr. Lennerz. As a result, only a small minority of kids and adults with type 1 diabetes really achieve satisfactory diabetes control even with all of the technology available today.
“Because of the breakthrough of insulin for diabetes, I think we forgot about nutrition in general for diabetes and we forgot about the low-carb approach,” she says. “It’s time we go back and explore what it can do for people with diabetes, especially those with type 1, where it has never truly been studied well.”
Small study showed benefits in type 1 diabetes
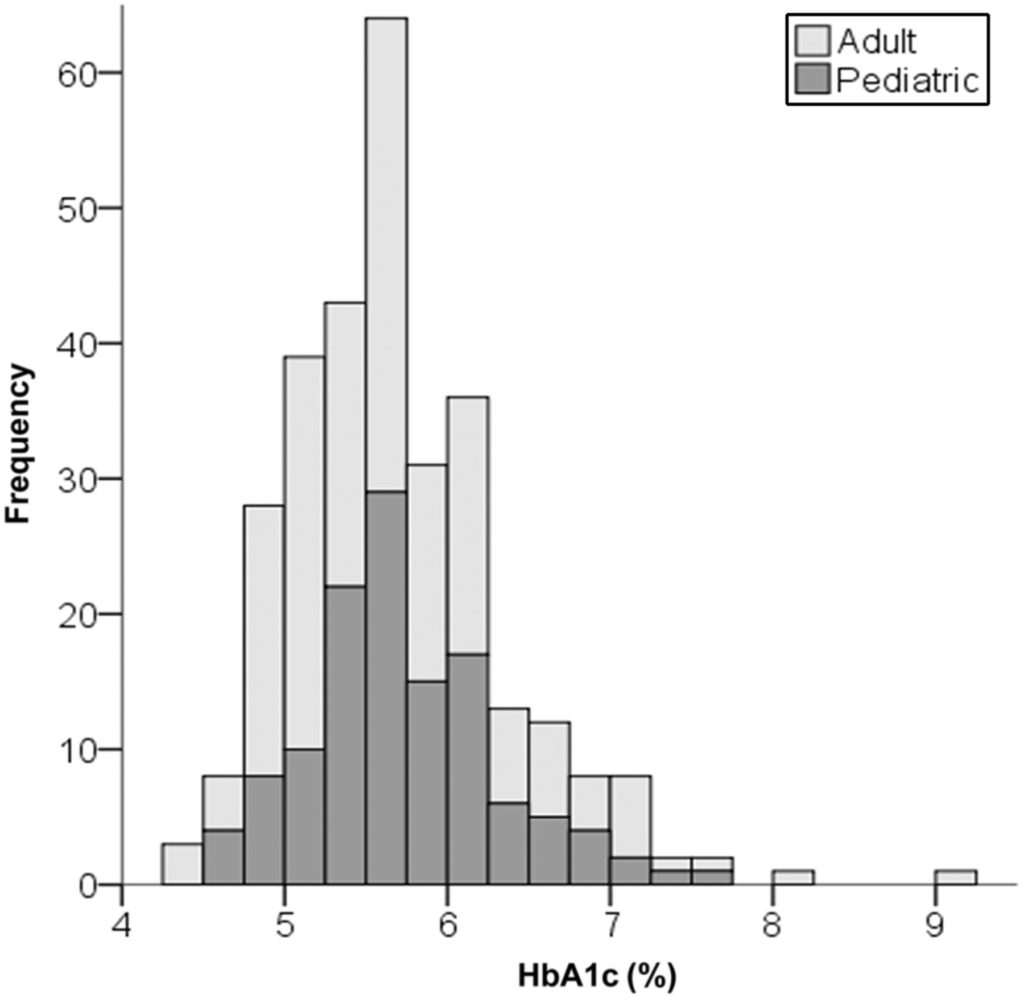
In 2018, Ludwig and Lennerz conducted their own study: a 300-participant survey looking at the effects of a low-carb diet in children and adults with type 1 diabetes. They found that the majority of those on the diet had HbA1C levels (a measure of blood sugar stability) in the normal range without many side effects.
“Plus, they needed less insulin, had fewer high or low blood sugar spikes, lower rates than expected of diabetes complications like hospitalizations and ketoacidosis, and high satisfaction with diet and diabetes control,” says Dr. Lennerz.
Buoyed by their own findings, Lennerz, Ludwig and colleagues advocate for high-quality, long-term clinical trials to determine whether this old dietary approach might help people with diabetes more effectively, and at a lower cost, than conventional treatment. “It’s more a question of rediscovering centuries-old wisdom, than the need for more technology,” says Dr. Ludwig.
Learn more about diabetes care at Boston Children’s Hospital
Related Posts :
-

Huge sequencing study links rare DNA changes to type 2 diabetes
Type 2 diabetes is a complicated disease influenced by genetics, lifestyle, and environment. Now, an international consortium of scientists has uncovered ...
-

Immune gene guards against type 1 diabetes by changing the microbiome. Do early antibiotics undercut its effects?
The health of our immune system is increasingly linked with the health of our intestinal bacteria. A mouse study from ...
-

Signs of diabetes and other medical emergencies: Don’t delay care during the COVID outbreak
Merlin Ladd had been home from school for about six weeks when his parents started to notice that something was ...
-

A toast to BRD4: How acidity changes the immune response
It started with wine. Or more precisely, a conversation about it. "My colleagues and I were talking about how some ...





