Kira’s story: how a diagnosis of fatty liver disease nourished a lasting lifestyle change
Kira’s journey with fatty liver disease began about six years ago, when imaging for other medical reasons showed areas of concern with her liver.
Fatty liver disease occurs when excess fat is stored in the liver; it can lead to progressive liver disease and is the most common pediatric liver disease in the country.
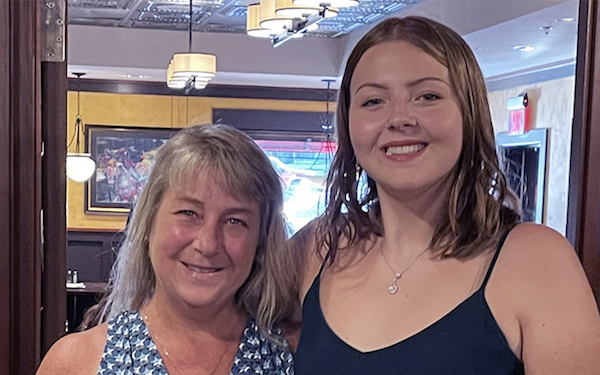
The diagnosis led Kira and her mom, Heather, to hepatologist Dr. Christine Lee, clinical nutritionist Leslie Mattimore, and others in the Fatty Liver Interdisciplinary Program at Boston Children’s Hospital, as well as to a new outlook on food, exercise, and a healthy lifestyle.
“I have to work with my body to help it make me better”
Fatty liver disease is associated with risk factors such as obesity and other metabolic conditions like type 2 diabetes, prediabetes, or high triglycerides. Kira didn’t have most of these co-occurring conditions, but she was overweight with a higher-than-recommended body mass index. So with the help of the team at Boston Children’s, Kira learned the impact that proper nutrition, portion control, and exercise have on her liver health and well-being.
“A diagnosis of fatty liver disease can be a real driver for families to make nutritional changes,” says Mattimore, who worked with Kira in the Fatty Liver Interdisciplinary Program.
“I’ve learned that I have to work with my body to help make me better,” Kira says.
Together, Mattimore, Dr. Lee, and Kira evaluated and adjusted Kira’s diet, exercise, and lifestyle habits. It turned into a family affair, with her mom joining in wholeheartedly.
Working together to win — and lose
Under the team’s guidance, Kira and her mom changed their diets, including reducing simple carbohydrates like white bread and sugar, incorporating more lean proteins, and being mindful of their portions. They also started a mother-daughter exercise regimen, going to the gym together three to four times a week.
Boston Children’s Hospital diagnoses fatty liver disease through a combination of imaging tests that may include ultrasound and FibroScan® — a specialized ultrasound machine designed to measure scarring and fatty change in the liver.
It took time for the pair to adapt to their new routine of healthier eating and exercise, but after a while, they began to notice the effects of their hard work. So did Kira’s care team.
Kira and her mom both lost significant weight, Kira’s fatty liver disease began to dissipate, and — most importantly to her mom — Kira’s self-esteem improved significantly.
“I have to commend my daughter,” her mom says. “Right from the beginning, she has taken this very seriously and has committed herself to getting better.”
Kira, now 16, credits the Boston Children’s team for helping her understand how food fuels her body and what she needs to eat to be healthy and strong, and she appreciates the team’s expertise and realistic approach to discussing food and nutrition.
“It’s difficult in the beginning — especially because it’s such a massive change,” Kira says about diet adjustments. “But it’s change that sticks with you.”
Mattimore says her job is often to start from scratch with families about the basics of food and nutrition.
“A lot of parents and families are burdened by outdated information about diets and nutrition,” she says. “So we set small goals that we work on each visit. They’re small changes but can be really difficult for many people.”
The biggest small changes Mattimore assigns patients are eliminating juice, soda, and sugary coffee and energy drinks, as well as eating regularly and not skipping meals.
A lifestyle for life
While weight loss is a huge motivating factor for many patients and families, both Mattimore and Dr. Lee emphasize that the strategies they help implement aren’t based on the numbers on the scale.
“We are not advising lifestyle changes just to make you look different,” Dr. Lee says. “The health of your liver and supporting your development as a growing person are why we’re involved. We’re trying to recalibrate how you look at food choices and to see what’s the healthiest for your organs. The byproduct of all this work just may happen to be changes in body proportions.”
Kira and Heather both appreciate this realistic and holistic approach.
“Dr. Lee was great about reminding us to be realistic,” Heather says. “She reminded Kira to give herself a break every once in a while.”
“I feel very lucky to have the results I’ve had,” Kira says. “Knowing about nutrition helps me think about the long-term: what do I want my older self to be like? It really puts it into perspective: the effects your diet can have.”
“This will be a lifestyle for her for the rest of her life,” Heather adds. “I’m thankful I’ve been able to go on this journey with her. We’ve found a lot of support in each other.”
Learn more about the how the Fatty Liver Interdisciplinary Program cares for children and young adults living with fatty liver disease.
Related Posts :
-

Partnering diet and intestinal microbes to protect against GI disease
Despite being an everyday necessity, nutrition is something of a black box. We know that many plant-based foods are good ...
-

Past patient outcomes could help single-ventricle surgery decisions
When considering whether a child who has a single-ventricle heart defect would benefit more from biventricular repair&...
-

Are weight-loss medications and surgery right for teens?
Advances in bariatric surgery and weight-loss medications have made weight management accessible to more adults. But are these approaches effective — ...
-

Addressing food insecurity and nutrition challenges in pediatric type 1 diabetes care
Managing type 1 diabetes can be overwhelming for children and families. As children learn to live with the disease, many cut ...





