A lot better than surgery: Jesse’s treatment for pectus excavatum

Like many growing boys, Jesse Zuniga went through a growth spurt when he was 12. Around that time, his pediatrician noticed an indentation in his chest. Neither he nor his mother, Sarah, had heard of pectus excavatum or vacuum bell therapy before. Soon they would be experts in both.
Also known as concave chest or funnel chest, pectus excavatum is a deformity of the chest wall. Instead of curving outward, the breastbone grows inward, causing an indentation in the middle of the chest. In many cases, pectus excavatum is mild and doesn’t require treatment. But the indentation can increase during periods of rapid growth, especially adolescence. If it becomes severe, surgery may be necessary.
Before his check-up, Jesse hadn’t given the shape of his chest much thought. “It was just what I knew,” he says. But after talking with his pediatrician, he and his mom, Sarah, decided to seek advice from a chest wall specialist.
Treatment options for pectus excavatum
At Boston Children’s Hospital, they met with Dr. David Mooney of the Pectus and Chest Wall Treatment Program. One treatment option would be to surgically reposition the inward-pointing bones in Jesse’s chest. But instead, Dr. Mooney suggested vacuum bell therapy, a non-invasive approach.
Vacuum bell therapy uses suction, created by a soft cup-shaped device and a hand pump, to slowly pull the breastbone forward. Patients wear the vacuum bell on their chest for several hours a day. The treatment typically lasts for a year or more.
“Jesse was young enough that the cartilage in his chest was flexible,” says Sarah. Starting the treatment at this stage of development increased his chances that vacuum bell therapy would work. And neither Jesse nor Sarah liked the idea of surgery. “We did some research and decided to give it a try.”
An ideal candidate for vacuum bell
Kelly Bartkus, a nurse practitioner in the Pectus and Chest Wall Treatment Program, took the lead in Jesse’s care. “Jesse was an ideal candidate for the vacuum bell,” says Bartkus. “He was just entering puberty, the best time for this therapy to work. I could tell that Jesse was eager to start therapy, and I had a good sense that he would take the therapy seriously and follow the regimen we prescribed.”
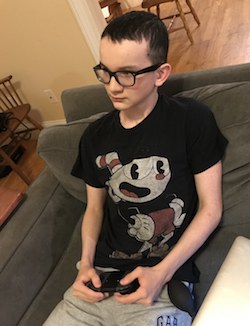
Jesse has worn the vacuum bell for several hours every afternoon for the past five months. He doesn’t pretend to enjoy it. The device is annoying, he says, but worth it. At a recent appointment at Boston Children’s, he and his mom got the great news that his chest had improved significantly. “For us, that was a motivator,” says Sarah. “To see that it’s actually working.”
Accepting temporary discomfort for long-term gain
Jesse has found ways to make the time pass while he wears the vacuum bell device. Video games and listening to music help. He also reminds himself of the bigger picture. “It’s something I have to do for now, and it’s a lot better than surgery.”
Sarah sees the vacuum bell as a positive learning experience for her son. “We all have to do some things we don’t want to do. Jesse has been so good about wearing the device. I’m very proud of him and glad he is seeing his efforts pay off.”
The vacuum bell will be a part of Jesse’s daily routine for at least another six months. He will continue to make routine office visits to the Pectus and Chest Wall Program, where Bartkus will monitor his growth and chest-wall changes. It remains to be seen if he’ll be able to put the device behind him after his current growth spurt, or if he’ll need to resume wearing it during future growth spurts. In the meantime, he sticks with his regimen and enjoys the progress he’s made so far.
Learn more about the Pectus and Chest Wall Treatment Program.
Related Posts :
-

“Observe. Be open.”: How Boston Children’s nurses are changing the future of global health
Ashley Birch, MSN, CPNP, a Boston Children’s pediatric nurse practitioner and Global Nursing fellow, didn’t expect a trash ...
-

Nurse-led innovations: A virtual-nursing pilot helps nurses thrive
It was night shift on the 9E Inpatient Medical Unit and Marisol Hernandez, BSN, RN, CPN, was helping another nurse ...
-

In a thriving gene therapy program, nursing leadership is the driving force
Gene therapy was made possible by decades of technological advances. But to execute gene therapy at scale? That would not ...
-

‘The reason I became a nurse’: Maeve’s memories of laryngeal cleft repair
Being a gastroenterology nurse is more than a profession for Maeve Lee. When she cares for patients with feeding tubes, ...





