Innovations in transcatheter valve replacement
The Cardiac Catheterization Program at Boston Children’s Hospital has been at the cutting edge of pediatric care for more than 60 years, developing and refining innovative catheterization techniques and procedures. “The program was built on a culture of collaboration, training, and innovation,” says Diego Porras, MD, FAAP, program chief. “We continue to foster new ideas and constantly strive towards improving and developing new approaches to care.”
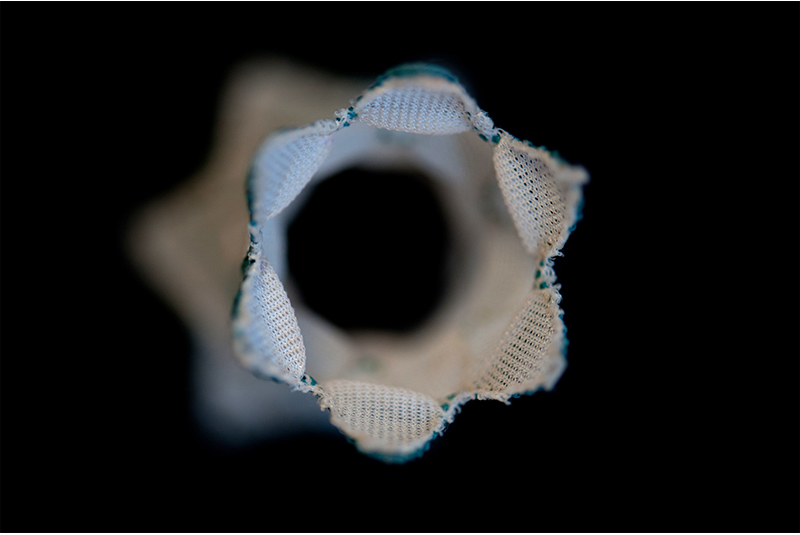
One particular area of robust development has been in transcatheter valve replacement, starting with the Melody valve in 2007 for replacement of the pulmonary valve. The team is continually looking for new ways to bring the benefits of transcatheter valve replacement to a wider range of patients.
Adapting off-label uses for valves
“In recent years, transcatheter valve replacement has exploded in the United States,” says Porras. “FDA approval, first of the Melody valve and then the SAPIEN valve, has given us more options. We’ve learned to adapt these valves for off-label use in other kinds of heart valves, as well as in progressively younger kids. We’re always seeing how we can push the envelope to use this technology in an ever-broadening spectrum of patients.”

For example, Porras says they started using transcatheter valve replacement in the mitral position in patients who already had a surgically placed valve. “We started placing the Melody or SAPIEN valve inside that valve, called a valve-in-valve procedure. That was very successful and seems to be working very well.” Over time, the team was able to further adapt this procedure for patients who don’t have a bioprosthetic valve, but who have a surgically placed annuloplasty ring (valve-in-ring) and even in the native mitral valve annulus in particular circumstances. This has allowed them to offer transcatheter valve replacement to patients who would not have been candidates a few years ago.
Porras says the goal of all these innovations is to avoid surgery. “Many of these patients have had a lot of surgeries, and every time you go back in to operate it’s risky, so if you can avoid two or three surgeries over a patient’s lifetime, that’s a significant benefit.”
Taking a multidisciplinary approach to innovation
The catheterization team also routinely collaborates with cardiac surgeons from the Heart Center on innovative treatment solutions for patients. One such collaboration involves using the Melody valve to replace the mitral valve in very small babies.
“When you have a mitral valve problem in an infant, there are not a lot of good options because most valves are designed for adults and very small valves tend to fail quickly as the child “outgrows” the valve, so these children often have many surgeries,” says Porras. “Dr. Sitaram Emani and the other surgeons started surgically placing a Melody valve for the mitral valve, and then we expand the surgically placed valve in the catheterization lab with a balloon as the child grows.”
Porras says they have performed many of these procedures over the years with good outcomes. “Now seven years out we are seeing that some of the leaflets are degenerating, and instead of operating again, we can place a new valve inside the surgically placed Melody valve in the cath lab. This is huge because it allows us to delay surgery in and allows the children to grow. Once they reach a size closer to adult size, we have better options for surgery.”
While many patients still require surgery, Porras says the goal is to continue to reduce the number of surgeries each patient requires over time to manage their congenital heart disease in an optimal way. “New advancements in technology will eventually allow more and more of our patients to get valves in the lab. While surgery will continue to be the cornerstone of management of complex congenital heart disease, we will continue to seek ways to manage these patients in a less invasive way.”
Learn more about the Cardiac Catheterization Program.
Related Posts :
-

Four things you should know about MAPCAs treatment
As the first grandchild in her family, Hannah Homan is in demand for frequent visits. She was also the focus ...
-

Treating MAPCAs with unifocalization surgery and cardiology care
Children born with a rare form of tetralogy of Fallot (ToF) face a challenging type of congenital heart ...
-

After surgeries to treat HLHS, Carter is healthy and happy at home in Florida
Carter Miller loves action. The 4-year-old Florida resident enjoys riding on golf carts and flying high on swing sets. ...
-

Advancing global health: Using AI to detect heart disease in children
In many low- and middle-income countries, pediatric cardiologists can’t help children with congenital heart conditions because of a critical ...





