Treating inflammation in MIS-C: An evidence-based approach

Multisystem inflammatory syndrome in children (MIS-C) is a complex, post-COVID-19 spectrum of illness that has affected a small number of children and adolescents. Symptoms can include features of Kawasaki disease, cardiac dysfunction, hypotension and toxic-shock-like signs, abnormal blood coagulation, and prominent GI symptoms. At its core is a hyperinflammatory response that we do not yet fully understand.
· A rheumatologist should be involved whenever MIS-C is suspected.
· Children with hyperinflammation (persistent fever and elevated inflammatory markers) may benefit from immunomodulators, especially if they have organ involvement.
· Based on the evidence, Boston Children’s is primarily using IV immunoglobulin, glucocorticoids, and anakinra.
Most children with MIS-C appear to have been previously healthy, with few or no prior COVID-19 symptoms. Most experts believe that the virus triggers immune dysregulation and hyperinflammation. To manage this inflammatory state, which can lead to multi-organ involvement, rheumatologists should be involved whenever MIS-C is suspected.
A working group at Boston Children’s Hospital has developed a treatment framework based on clinical observations, a handful of published reports and ongoing studies, and results of treatment trials for other inflammatory conditions, including macrophage activation syndrome and hemophagocytic lymphohistiocytosis (HLH). The approach is evolving over time as more is learned about MIS-C.
Immunomodulators in MIS-C
Children with hyperinflammation have persistent fever, markedly elevated inflammatory markers (such as C-reactive protein, D-dimer, and ferritin), and elevated proinflammatory cytokines (such as IL-1 and IL-6).
Because MIS-C is an entirely new condition, we are treating patients with medications that are effective in other inflammatory syndromes and have a safe side effect profile.”
– Lauren Henderson
“We are using immunomodulators in this group of patients,” says Boston Children’s rheumatologist Lauren Henderson, MD, MMSc. “Because MIS-C is an entirely new condition, we are treating patients with medications that are effective in other inflammatory syndromes and have a safe side effect profile.”
The goal of using immunomodulators in MIS-C is to prevent progression to shock, reduce the need for ICU admission or organ support, and prevent coronary artery dilation and aneurysms.
“If a patient has symptoms suggestive of MIS-C, we try to treat them fairly aggressively early on, to avoid decompensation,” says Boston Children’s immunologist Douglas McDonald, MD, PhD.
Choosing a treatment
The most common anti-inflammatory treatments for MIS-C at Boston Children’s have a track record of safe use in children in the setting of infection. Outcomes are being closely tracked at Boston Children’s and internationally.
IV immunoglobulin (IVIG) is a standard first-line treatment for Kawasaki disease to protect the coronary arteries from inflammation, and has been used for decades in immune deficiencies, autoimmune problems, and persistent infections. IVIG is now also used in MIS-C even when there are no clear Kawasaki-like features, although it’s still not clear how much benefit it provides.
Glucocorticoids (methylprednisolone, prednisone, prednisolone, dexamethasone) offer general immune suppression. They are often used in conditions such as shock, acute respiratory distress syndrome, Kawasaki disease, and other inflammatory conditions. Some studies in patients with MERS and SARS showed that the use of glucocorticoids delays viral clearance, and there is some concern that this could also occur in patients with SARS-CoV-2. However, children with MIS-C present late in the infection and test positive for SARS-CoV-2 IgG, suggesting that they have developed an antibody response and that clearig the virus may not be the primary problem in MIS-C.
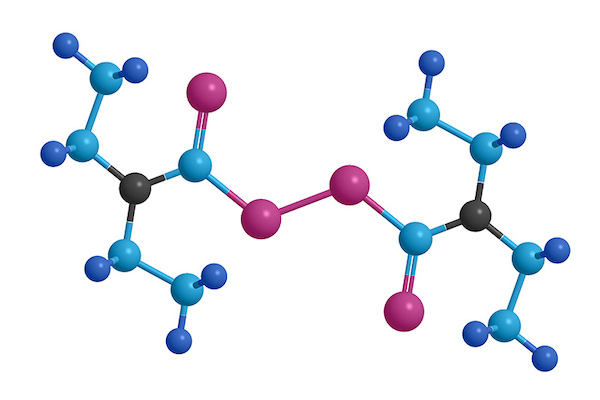
Anakinra is among several biologic drugs that target specific inflammatory cytokines, based on laboratory findings. It targets IL-1ß, which appears to have an important role in cytokine storm syndrome. Originally developed for rheumatoid arthritis, anakinra has been used in a variety of other inflammatory conditions. A recent uncontrolled study in adults with COVID-19, published May 7 in Lancet Rheumatology, found it to be associated with clinical improvement.
“There are studies indicating that anakinra is relatively safe in severe infections, including sepsis,” says Henderson. “It has a short half-life, so can be discontinued rapidly if it’s not effective or if there are side effects. In addition, it has been used safely in children for conditions such as systemic juvenile idiopathic arthritis for many years.”

Other immunomodulators being used for MIS-C
So far, patients with MIS-C at Boston Children’s have done well with these treatments. Clinicians around the world are trying various other immunomodulators.
Canakinumab, a monoclonal antibody also targets IL-1, but has a longer half-life.
Tocilizumab, mainly studied in adults to date, targets the cytokine IL-6. “We don’t have much experience with tocilizumab in the setting of severe infections, even in adults, so we are not using it as first-line treatment at Boston Children’s Hospital,” says Henderson.
JAK inhibitors, developed for rheumatoid arthritis,block a pathway that turns on multiple cytokine genes. However, there are few data on their safety in the setting of severe infection. In a recent uncontrolled study, 12 adults with mild to moderate COVID-19 given the JAK inhibitor baricitinab showed a marked improvement.
“Rather than using 1L-1 or IL-6 blockade or a lot of steroids, we can hit many cytokines at once,” says Boston Children’s rheumatologist Mary Beth Son, MD. “But that’s really untested territory.”
Not everyone needs immunomodulators
Some immunologic treatments, such as IVIG, may be in short supply, while others are very expensive. And not all patients with MIS-C need them.
On the horizon
Labs around the world are exploring other immunomodulatory approaches to COVID-19 inflammation in both children and adults. At Boston Children’s, a study led Judy Lieberman, MD, and Hao Wu, PhD, found that disulfiram, a drug used to treat alcoholism, blocks formation of the pores through which cells release IL-2 and other cytokines.
Another study led by Raif Geha, MD, and Janet Chou, MD, is exploring the role of endoplasmic reticulum (ER) stress in COVID-19. In a mouse model, a drug that reduces ER stress also reduced levels of certain cytokines.
“Most patients identified to date with MIS-C have been more severe, many of them in the ICU,” says Henderson. “But there are probably children who are much more mildly affected, with just a fever and rash, and may only need observation.
“We don’t know much about this group yet, but if a child is doing fairly well, does not have low blood pressure or severe abdominal pain, and does not have greatly elevated markers of inflammation, it might be reasonable to monitor them as outpatients with lab work and echocardiograms.”
Son agrees. “There should be some sort of organ involvement; fever and inflammation on their own may not require immunomodulator treatment.”
However, children will require close follow-up with a cardiologist and rheumatologist, since it’s still unclear which children are at risk for bad outcomes such as coronary artery aneurysms or heart block.
More study needed
According to the World Health Organization, more than 1,000 children worldwide have been treated for MIS-C based on clinicians’ best guesses. To capture their outcomes and inform future clinical trials, the WHO has launched the Best Available Treatment Study. Although this study isn’t randomized, its strict methodology will allow patients to be retrospectively matched for severity. The study should inform the results of future randomized trials.
As of early May, the nationwide Overcoming COVID-19 study, led by Adrienne Randolph, MD, MSc, a critical care physician at Boston Children’s, has been capturing real-time data on MIS-C.
Much more needs to be understood about the spectrum of illness in MIS-C. That includes which presentations portend bad outcomes, what factors contribute to risk, which medications work best, and how children with mild and severe MIS-C fare long-term.
“We need clinical trials,” says Son. “It’s never good to work on anecdote, but that’s the space we’re in for now.”
Read more about clinical care for COVID-19 and visit the Rheumatology Program at Boston Children’s Hospital.
Related Posts :
-

Promising advances in fetal therapy for vein of Galen malformation
In 2024, Megan Ingram* of California and her husband were preparing for the birth of their third child when a 34-week ...
-

The hidden burden of solitude: How social withdrawal influences the adolescent brain
Adolescence is a period of social reorientation: a shift from a world centered on parents and family to one shaped ...
-

A toast to BRD4: How acidity changes the immune response
It started with wine. Or more precisely, a conversation about it. "My colleagues and I were talking about how some ...
-

A unique marker for pericytes could help forge a new path for pulmonary hypertension care
Pulmonary arterial hypertension (PAH) is a rare condition that’s difficult to treat. The hallmarks of the disease — narrowing of ...





