Which genetic syndromes can increase a child’s risk of cancer?
Inherited cancers account for at least 5 to 10 percent of all pediatric cancers. The same advances in technology that have enabled scientists to decode the human genome now allow doctors to determine when a child has been born with an error (mutation) in a specific gene that puts them at increased risk of childhood cancer.
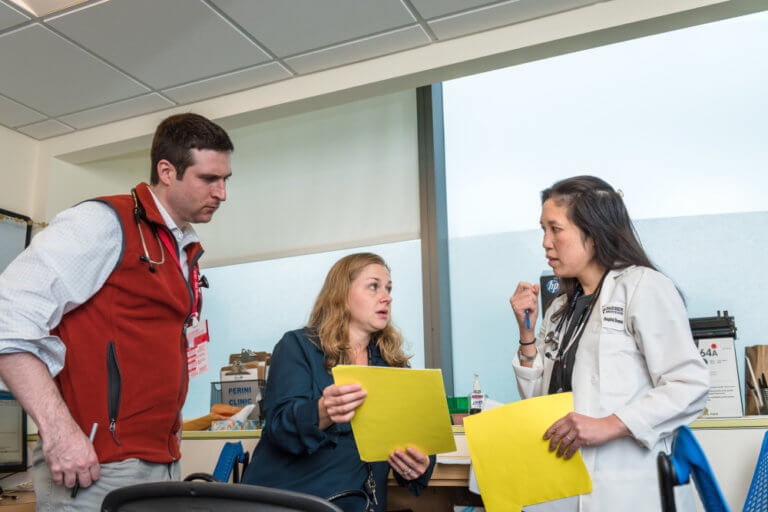
Researchers have identified over 100 genes that can cause specific cancer predisposition syndromes if a mutation is present. “A child who is born with a mutation in one of these genes may be at higher risk of developing a tumor over their lifetime,” says Dr. Junne Kamihara, co-director of the Pediatric Cancer Genetic Risk Program at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center. “Knowing this risk can help empower patients, their families, and their care providers.”
Genetic predisposition syndromes
Some examples of genetic predisposition syndromes affecting children include:
- Li-Fraumeni syndrome (LFS), which is caused by a mutation in the TP53 gene. Children with LFS are at risk of developing a wide range of cancers — including adrenal gland cancers, brain tumors, sarcomas, and leukemias — often at early ages. People with LFS also have higher risks of developing cancer as adults, including breast cancer, colon cancer, and others.
- Hereditary retinoblastoma, which is caused by a mutation in the RB1 gene. Children who are born with an RB1 mutation have high risks of developing tumors in the retina, the part of the eye that receives light input. This rare cancer is usually diagnosed in children under age 5. People with RB1 mutations also have a higher risk of developing other cancers later in life, including bone cancers, soft tissue cancers, melanomas, and other tumor types.
- DICER1 syndrome, which is caused by a mutation in the DICER1 gene. Children with DICER1 syndrome have a higher risk of developing pleuropulmonary blastoma, a rare lung tumor that is usually detected early in life. Children may also develop tumors in their kidneys, ovaries, thyroid, and other organs.
- Familial adenomatous polyposis (FAP), which is caused by a mutation in the APC gene. A classic mutation in APC may result in the formation of hundreds to thousands of polyps in the colon that may begin forming in late childhood to the teen years. These patients have a higher risk of developing colorectal cancer.
- Multiple endocrine neoplasia (MEN) type 1 and type 2, which is caused by a mutation in the MEN1 (for type 1) or RET gene (for type 2). Mutations in the MEN1 gene increase the risk of developing tumors in several of the body’s hormone-producing endocrine organs, such as the parathyroid glands, pituitary gland, and pancreas. Mutations in the RET gene increase the risk of medullary thyroid cancer. These tumors can occur in childhood and adulthood.
- von Hippel-Lindau syndrome (VHL), which is caused by a mutation in the VHL gene. Children and adults with VHL are at risk of developing tumors and cysts that grow in different parts of the body, especially the brain, spine, eye, kidneys, pancreas, and genital tract.
Genetic testing
Genetic testing to look for these syndromes and others can serve a vital proactive role in a child’s health. As part of the Pediatric Cancer Genetic Risk program at Dana-Farber/Boston Children’s, families meet with a genetic counselor to assess the family history and offer genetic testing.
“If there is a known gene mutation in the family, for example, we can look for the gene mutation. If it is found in the child, we can proactively take measures for early detection,” explains Kathy Schneider, one of the senior genetic counselors in the program.
For example, if a mother carries an RB1 mutation, then her child could be tested for the same mutation at birth (or even prenatally). Children who carry the RB1 mutation would be closely monitored with frequent eye exams to detect any tumors at their earliest stages. This can help to preserve vision and the eye.
If a child is already being treated for cancer, genetic screening for syndromes can still provide the care team with invaluable information. “Genetic testing can help to inform risk for second primary tumors, help to inform treatment, and direct testing and care for siblings and other relatives,” Dr. Kamihara says.
As the field continues to evolve, Dr. Kamihara is optimistic about the future. “Someday I hope that we can not only work on finding cancers early, but also prevent these cancers before they even occur,” she says. “No child should develop cancer, and we should be doing everything we can to make this a reality.”
Learn more about the Pediatric Cancer Genetic Risk Program.
Related Posts :
-

Making genome sequencing a first-line test in rare disease
Children with rare diseases often undergo years of medical visits and genetic testing before they get a diagnosis. Over the ...
-

Boosting vaccines for the elderly with ‘hyperactivators’
As we age our immune systems start to flag, leaving us more susceptible to cancer and infections — and less responsive ...
-

Two rising stars in kidney genetics: Nina Mann and Amar Majmundar
A healthy, functional kidney must maintain a delicate balance of water, nutrients, and electrolytes so it can properly filter the ...
-

Whether she’s embracing school, sports, or music, Lindsey shows how Williams syndrome can be managed
One of the first things Lindsey Franco will tell you is, “I like being me. I like being happy.” The 19...