Doing everything possible for Gabby: A team approach to short bowel syndrome

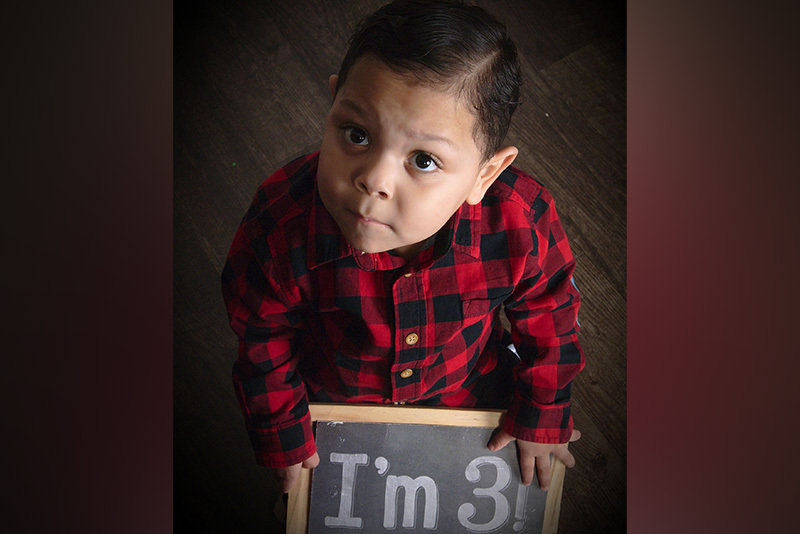
Gabriel “Gabby” Lopez loves everything hot and spicy. “He will eat a ghost pepper without hesitation,” says his mother, Mayra. “He eats more spicy food than a grown man.” It’s an impressive feat, not only because Gabby is just 3 years old, but also because he has spent the majority of his life receiving his nutrition through a central line and G-tube.
Born prematurely at 26 weeks, Gabby weighed just over 2 pounds. When he was 2 weeks old, he developed necrotizing enterocolitis, a serious illness that leads to the death of a baby’s intestinal tissues. As a result, he lost about 80 percent of his intestines and developed short bowel syndrome. In this condition, the body can’t absorb the nutrients to grow and thrive, and many children must receive nutrition intravenously through a central line (total parenteral nutrition, or TPN) or through a feeding tube.
“It’s scary to be told your child only has 20 percent of his intestine left,” remembers Mayra. “I could tell from the look on his doctors’ faces that they didn’t think he would be okay.”

A team approach to short bowel syndrome
Those same doctors recommended that Gabby and his parents travel to a specialized children’s hospital, which eventually brought them to the Center for Advanced Intestinal Rehabilitation (CAIR) at Boston Children’s Hospital. “We liked that CAIR offered Omegaven,” says Mayra. This fish oil-based drug — now FDA-approved to treat liver disease associated with the use of TPN in children — was developed at Boston Children’s.
Arriving in Boston from Queens, New York, the family felt a new sense of hope. “At CAIR, they told us they would do everything possible for Gabby,” says Mayra. That has entailed surgery by Dr. Biren Modi to remove a blockage, nutritional help, and a group of dedicated clinicians including nurse practitioner Elizabeth Castle, Drs. Christopher Duggan and Alexandra Carey, and social worker Jessica McCaig. “We love that we have a whole team here to support us,” says Mayra. “At any given time, they’re just a phone call away.”
Grateful for every milestone
Much of that support has come in the form of helping Gabby’s parents navigate his care. Although many kids with short bowel syndrome can appear perfectly healthy, Mayra knows just how much work goes on behind the scenes. From flushing his central line and preparing infusions, to changing his dressings and more, taking care of a child with this condition can seem like a full-time job. “You almost feel like a nurse sometimes,” she says. “But the CAIR team makes it look easy. They taught us everything from A to Z, and now it’s become second nature.”
Today, Gabby has overcome an initial oral aversion and now enjoys eating by mouth while still relying on his central line for supplemental nutrition. He loves listening to music, making art, and taking baths. His journey hasn’t always been easy: “Sometimes it feels like we’re taking two steps forward and six steps back,” says Mayra, who is active in support groups for parents of kids with short bowel syndrome. “But everyone’s path is different and we’re grateful for every little milestone.”
Learn about the Center for Advanced Intestinal Rehabilitation
Related Posts :
-

Genetic causes of congenital diarrhea and enteropathy come into focus
Congenital diarrheas and enteropathies are rare and devastating for infants and children. Treatments have consisted mainly of fluid and nutritional ...
-

Then and now: Catching up with some of our short bowel syndrome kids
Also known as “short gut,” short bowel syndrome is a life-threatening condition in which a lack of functioning intestine can ...
-

Catching up with Lucas eight years after his multivisceral transplant
Lucas and his mom, Heather, aren’t shy talking about his health journey and his multivisceral transplant. “If other families ...
-

Studies pinpoint risk factors for complications of pediatric intestinal failure
Pediatric intestinal failure occurs when patients lack the amount of intestine necessary for growth and development. As advances in treatment ...





