Taking a sideswipe at high-risk neuroblastoma
Cancer and other diseases are now understood to spring from a complex interplay of biological factors rather than any one isolated origin. New research reveals that an equally-nuanced approach to treating high-risk neuroblastoma may be the most effective way to curb tumor growth.
One challenge in treating pediatric cancers like neuroblastoma is that they are not initiated from the same kinds of genetic mutations as adult cancers, which usually arise from mutations related to an accumulation of DNA replication errors or environmental factors. In contrast, childhood cancers more often stem from genetic duplications, deletions or translocations, the latter of which occurs when a gene sequence switches its location from one chromosome to another.
On top of this, pediatric cancers that develop from these types of genetic alterations often involve genes called “transcription factors”, which encode for production of proteins that regulate the transcription of specific DNA sequences.
“Transcription factors have been notoriously difficult to make drugs against and they are frequently translocated or amplified in pediatric cancers,” says Kimberly Stegmaier, MD, who is co-director of the pediatric hematologic malignancy program at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center and also a member of the Broad Institute’s Cancer Program.
A tale of two neuroblastoma genes
In pediatric high-risk neuroblastoma, for example, a transcription factor known as MYCN becomes amplified with many copies inside each cancer cell. So far, it has not been possible to target MYCN pharmacologically.
But now, a team led by Stegmaier has discovered a roundabout way to stave off the effects of MYCN amplification through a link with another gene, called EZH2. Their findings were published this month in the Journal of Clinical Investigation.
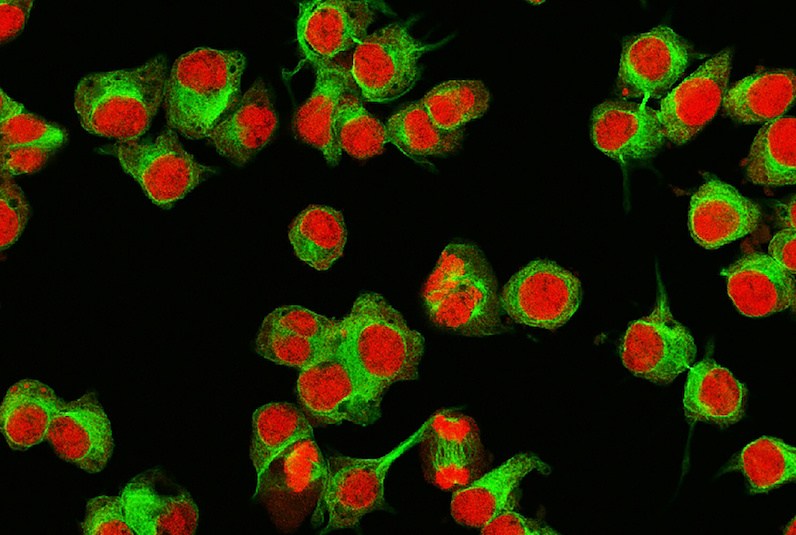
In their experiments, the team found that the MYCN protein directly controls the expression of the EZH2 gene, which encodes for the EZH2 protein, a known tumor cell proliferator across various types of cancers. When MYCN is amplified, over-production of the EZH2 protein blocks tumor suppressor activity and normal differentiation programs in the neuroblastoma cells and prevents them from growing into mature neurons, according to a story about the research by the Broad.
Strikingly, by blocking EZH2 through genetic repression and chemical inhibitors, the researchers were able to impair neuroblastoma growth.
Setting the stage for a clinical trial
The findings are all the more interesting because an EZH2 inhibitor is already being evaluated in children with certain cancers.
Called tazemetostat, it’s being clinically tested in two studies led by Susan Chi, MD, of Dana-Farber/Boston Childrens: A phase 1 clinical trial for children with certain relapsed/refractory malignancies and a phase 2 nationwide precision medicine study sponsored by the National Institute of Cancer (NCI) and the Children’s Oncology Group (COG).
“Given these initial findings with other EZH2 inhibitors, we are now evaluating tazemetostat as a potential molecule to treat MYCN-amplified neuroblastoma,” says Stegmaier. “It is my hope that our publication and a growing body of other data supporting the role of EZH2 in high-risk neuroblastoma will fuel the development of a clinical trial to test EZH2 inhibitors for the treatment of children with this type of cancer.”
Related Posts :
-

New research sheds light on the genetic roots of amblyopia
For decades, amblyopia has been considered a disorder primarily caused by abnormal visual experiences early in life. But new research ...
-

Thanks to Carter and his family, people are talking about spastic paraplegia
Nine-year-old Carter may be the most devoted — and popular — sports fan in his Connecticut town. “He loves all sports,” ...
-

A new druggable cancer target: RNA-binding proteins on the cell surface
In 2021, research led by Ryan Flynn, MD, PhD, and his mentor, Nobel laureate Carolyn Bertozzi, PhD, opened a new chapter ...
-

Forecasting the future for childhood cancer survivors
Children are much more likely to survive cancer today than 50 years ago. Unfortunately, as adults, many of them develop cardiovascular ...





