Innovative POEM procedure gives Emma an option for achalasia
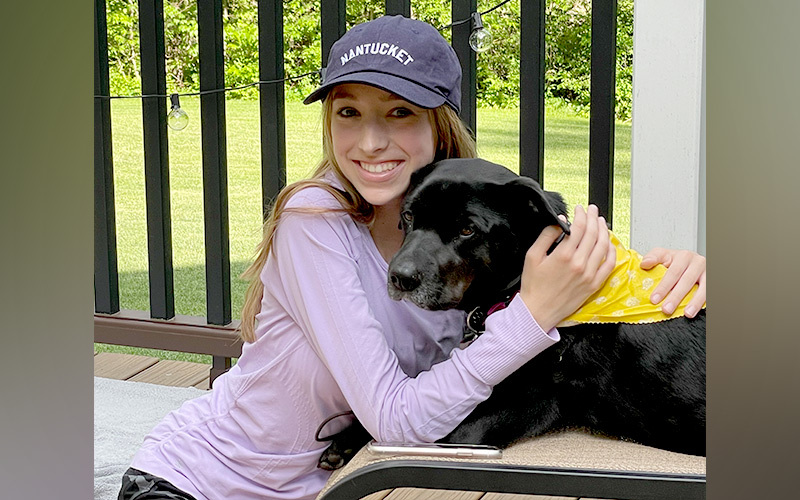
Like a lot of teenagers, Emma Reiner loves pizza — so it shouldn’t have been a surprise when she recently enjoyed four slices in one sitting. But for Emma, the meal was an accomplishment. For more than a year, she had felt nauseous after taking just a few bites of food. “It felt like the food wouldn’t go down,” she remembers. “I tried drinking more water and taking TUMS, but nothing helped.”
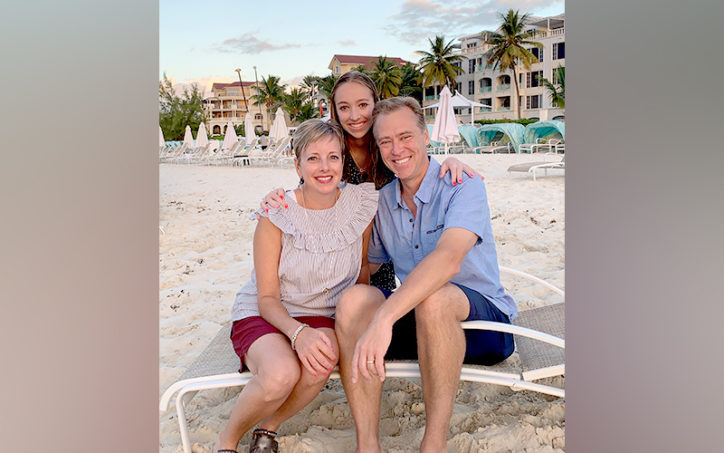
When a course of the proton pump inhibitor Prilosec didn’t help either, her parents, Melissa and Jeremy, knew it was time to seek more specialized care. In September 2020, Dr. Samuel Nurko, director of Boston Children’s Motility and Functional Gastrointestinal Disorders Center, diagnosed Emma with achalasia, a rare disorder of the esophagus that makes swallowing difficult.
Exploring options for achalasia
Although the Reiners were glad to have an answer, the diagnosis was still unnerving. “As parents, to have never heard of achalasia and then to learn that it was incurable was shocking,” says Jeremy. But knowing that the problem is treatable eased their concerns a bit. In fact, Emma had three treatment options to choose from.
The first, which would involve dilating her esophagus, didn’t sound like it would be effective enough. The second option, a more invasive surgical procedure called myotomy, would widen Emma’s esophagus, but came with a longer recovery period. Emma, a competitive swimmer, worried that the downtime would affect her upcoming season.

Learning about POEM
Then, the team told the Reiners about a third procedure that might be the right fit. Called peroral endoscopic myotomy (POEM), this innovative approach offers a less-invasive way to perform myotomy with similar outcomes, shorter hospital stays and recovery times, and without skin incisions or surgical access points through the chest wall. POEM has been used for over a decade to treat adults, but Dr. Peter Ngo is the first pediatric gastroenterologist in the U.S. to perform it in older children and teens.
At first, the family was a little nervous about the procedure. “Dr. Ngo explained what to expect and offered to connect us with parents of other patients who had undergone POEM,” says Melissa. Emma felt comfortable with the decision, too. “I knew it was the best choice,” she says.

Getting back to normal
Now, just two months after the procedure, Emma is feeling better than ever. After a week of liquids and soft foods, she’s been able to eat normally again — including those slices of pizza. Even better, she can eat before her evening swim practices, which achalasia made challenging. And she hasn’t experienced chronic acid reflux, which can be a risk of POEM for some patients.
“Everyone at Boston Children’s was fantastic,” says Jeremy. “We’re so happy that Emma can get back to a more normal lifestyle.”
Learn more about acahalsia and esophageal motility disorders, as well as POEM and other treatments offered by the Division of Gastroenterology, Hepatology, and Nutrition.
Related Posts :
-

Dysmotility may play a major role in respiratory symptoms
Clinicians whose patients exhibit respiratory symptoms frequently assume that gastroesophageal reflux disease (GERD) is responsible. However, esophageal and gastric dysmotility ...
-

‘Never stop looking for answers’: Andrea’s journey with dysmotility
As a volunteer at Caritas Internationalis, Andrea Hernandez loves helping feed the hungry. Yet, until recently, Andrea herself was unable ...
-

Swallowing problems: 4 things to know about dysphagia
It seems like second nature to most of us, but swallowing is actually an intricate process with multiple stages, from ...
-

Ready for the next step: Innovative care for Chase
Chase Essex loves pizza and has even prepared shrimp scampi for his family. So it might come as a surprise ...





