Detecting shunt failure in hydrocephalus without imaging or surgery: ShuntCheck
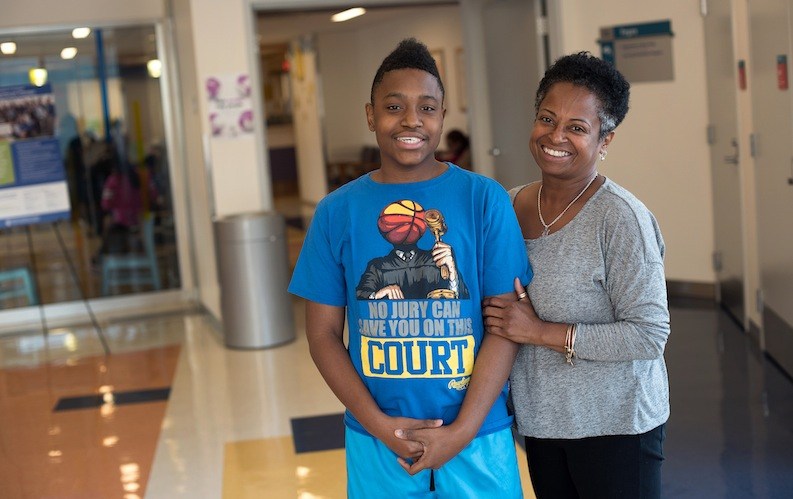
Antonio Venus-Reeve, 14, had his first shunt surgery for hydrocephalus when he was 2½ months old. Born at 25 weeks’ gestation, weighing less than two pounds, he had a serious brain bleed seven days later.
As Antonio’s head began to swell with excess fluid, neurologists at Boston Children’s Hospital told his mother, Joanne Venus-Williams, that Antonio probably would not be able to walk, talk or develop major motor skills. “Neurosurgery got involved and the team did daily spinal taps to draw out the fluid in his brain,” says Venus-Williams. “They were hoping he wouldn’t need a shunt, but we got to the point where we knew it was the way to go.”
The shunt — a tube placed in the brain — would drain the excess fluid into Antonio’s abdomen. Before it was placed, neurosurgeon Joseph Madsen, MD, came to see Antonio. Joanne recognized him: years earlier, Madsen had been the chief neurosurgical resident at Massachusetts General Hospital where Joanne had coordinated the neurosurgery clinic. “I felt confident that my son was in good hands,” Joanne says. “Even at a young age, Dr. Madsen had his head on.”
But the shunt was only the beginning of Antonio’s fight. Shunts have a tendency to plug up and malfunction, requiring surgery to correct or replace them.
Antonio’s first shunt failure occurred before he was 1½. It was always hard to tell when his shunt stopped working: He’d become lethargic, tired, not eating, crying — symptoms that could be caused by anything. “Do we take him to the hospital or not take him to the hospital?” says Joanne. “That was always an issue.”
The shunt shuffle
Rushed to the hospital countless times, Antonio has undergone countless CT and MRI scans of his brain to check his shunts. The CT scans exposed him to radiation, and the MRI scans, as they were done in those days, required him to lie still inside a scanner, taxing for a child and requiring sedation.
Even worse, imaging can’t always show whether a shunt is failing. That meant a lot of exploratory surgery, sometimes leading to a repair, sometimes not. The problem was multiplied when Antonio had a second shunt implanted. Joanne estimates he’s had 16 or 17 surgical procedures related to shunts during his lifetime.

“Now, when he gets headaches, has a very low heart rate and has trouble breathing, we know it’s a shunt problem, but we can’t tell which shunt is failing and which to repair,” says Joanne.
The ice cube test
Madsen had been concerned about the problem of detecting shunt failure for years — especially the false alarms. About a decade ago, at a conference, he met another neurosurgeon, Samuel Neff, who was trying to solve the same problem for his nephew Spencer.
Neff’s idea was to chill the fluid within the shunt by placing an ice cube over it. Clinicians could then test for a drop in temperature downstream of the shunt, which would indicate the shunt was patent — meaning that fluid was flowing through it. Neff made prototypes in his home shop, with algorithms to interpret temperature changes in the skin over the shunt. He then tested his invention on Spencer.
Madsen approached Neff and ultimately became inventor of part of the system, now known as ShuntCheck. In 2011, a small biotech called NeuroDx (Princeton, NJ) received a $3 million NIH grant to develop and test the device.
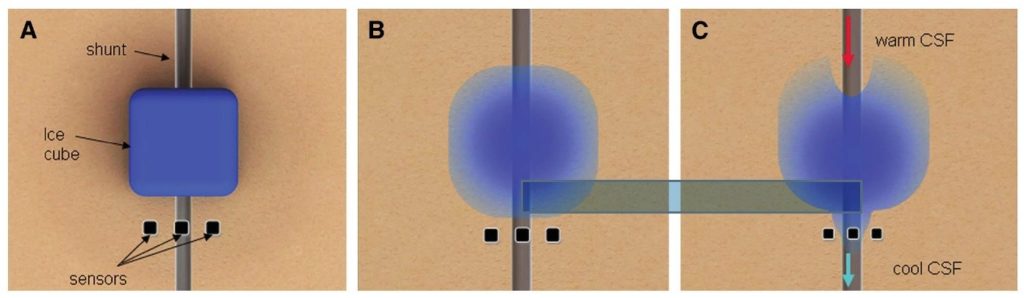
Madsen led the testing, and Antonio was part of the study. The researchers discovered that flow in shunts naturally waxes and wanes, making it difficult to distinguish a blocked shunt from a patent shunt by thermal flow detection. At Madsen’s suggestion, NeuroDx solved the problem by adding a mechanism called the MicroPumper that vibrates the shunt, accelerating flow temporarily for test purposes.
Checking ShuntCheck
Earlier this year, at the American Society of Pediatric Neurosurgeons meeting, Madsen presented data from a 10-hospital study of 348 shunt patients who were evaluated with ShuntCheck/MicroPumper and brain CT or MRI.
ShuntCheck/MicroPumper, combined with imaging, identified shunt blockage in 44 of 52 confirmed cases, giving it a positive predictive value of 84.6 percent, versus 64.5 percent for imaging alone. In patients whose shunts weren’t blocked, ShuntCheck/MicroPumper, combined with imaging, appropriately ruled out blockage in all of them — a negative predictive value of 100 percent, versus 93.9 percent for imaging alone.
When patients were assessed by their attending physicians before diagnostic testing was completed, 193 were judged to be “unlikely to require surgery.” ShuntCheck/MicroPumper ruled out shunt blockage in 90 of these patients, with 100 percent accuracy. The investigators calculate that ShuntCheck could have spared 86 scans, 33 hospital admissions for observation and 16 invasive tests for patients without shunt failure.

“Since patients were tested with ShuntCheck before the clinical team had decided what to do,” says Madsen, “the device might be able to sharpen our clinical decision-making and give us more confidence in sending patients home from the emergency department.”
Another arm of the study, using ShuntCheck without the MicroPumper, showed equally good results, the team found.
Antonio the fighter
NeuroDx received U.S. FDA 510(k) premarket notification clearance for ShuntCheck in 2013, meaning that it is clinically available to physicians.
Spencer, the first patient to test the device, reports that he’s doing great; he’s graduated from college and is now an aspiring sportswriter.
As for Antonio, he has beat the odds. Between his shunts, Early Intervention services and Joanne’s sheer determination, he learned to walk and ride a bike and today attends an inclusionary program at school. His last shunt surgery was in December.

Although any head injury — even a minor one — would be a threat, Antonio swims, rides his bike and plays basketball. “I got to the point where I said, “it’s not fair to limit this child,” says Joanne. “He’s a little boy, let him live his life. It’s a quality of life issue. Whatever he feels like he can do, I let him do.”
This hasn’t been without consequences: Once, trying to do a wheelie on his bike, Antonio shattered a valve on his shunt. But Joanne has learned to let go.
“We don’t know how much time Antonio has,” she says. “It’s a day to day battle, and we don’t know from today to tomorrow whether his shunts are going to fail. If they fail, he might not make it. Any research that Dr. Madsen does, we try to be available. We want to help so other children with hydrocephalus can have a better chance.”
Related Posts :
-

Promising advances in fetal therapy for vein of Galen malformation
In 2024, Megan Ingram* of California and her husband were preparing for the birth of their third child when a 34-week ...
-

The hidden burden of solitude: How social withdrawal influences the adolescent brain
Adolescence is a period of social reorientation: a shift from a world centered on parents and family to one shaped ...
-

A toast to BRD4: How acidity changes the immune response
It started with wine. Or more precisely, a conversation about it. "My colleagues and I were talking about how some ...
-

A unique marker for pericytes could help forge a new path for pulmonary hypertension care
Pulmonary arterial hypertension (PAH) is a rare condition that’s difficult to treat. The hallmarks of the disease — narrowing of ...





