COVID-19 and surgery: Lessons in safety
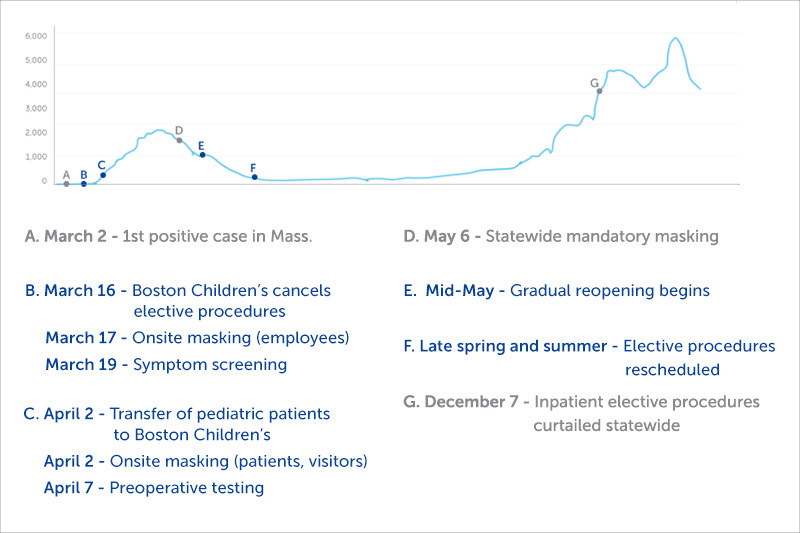
When Massachusetts recorded its first COVID-19-positive test result in early March 2020, health officials knew little about the virus. They didn’t know, for instance, how it was transmitted or how to protect patients and clinicians during surgical procedures.
In the weeks that followed, Boston Children’s Hospital made several difficult but necessary decisions. We cancelled elective surgical procedures and temporarily closed several of our satellite locations. We modified many of our clinical practices and the way clinicians interacted with patients to reduce the chance of transmission. Based on infection trends worldwide, we instituted a policy of mandatory masking several weeks before Massachusetts issued a statewide order.
Massachusetts is now in the midst of a second COVID-19 surge. This time, however, we know far more about the virus and preventing transmission. While the hospital’s priorities remain the same — ensuring safety and providing the best possible care — the lessons of 2020 have enabled Boston Children’s to continue delivering care during the current outbreak.
Lesson 1: Safety takes time and patience
In the early days of the pandemic, with little access to COVID-19 testing, Boston Children’s surgical teams had no way to know if their patients were infected. “At first, we had to treat every patient as if they were positive,” says Surgeon-in-Chief, Steven Fishman, MD.
Members of the hospital’s Biocontainment Unit spread out, training colleagues in heightened infection-control measures: airway management, patient transportation, and proper donning and doffing of personal protective equipment (PPE). Since it was first established in 2014 during the Ebola outbreak in Africa, the Biocontainment Unit had spent six years developing best practices for the care of highly infectious patients.
In another part of the hospital, our Simulator Program tested new COVID-19 precautions and quickly recognized that some guidelines were impractical under urgent conditions. The team refined any such guidelines, rolling them out only after demonstrating they could work in a live clinical environment.
Other teams went to work establishing in-house COVID-19 testing capabilities and drive-through testing. By early April, all patients scheduled for surgery underwent COVID-19 testing the day before their procedure.
Lesson 2: We are all in this together
Early trends in New York and Washington state suggested that adult hospitals could soon be overburdened by COVID-19 cases, while children’s hospitals would probably not. Boston Children’s was designated the pediatric hospital for New England. As COVID-19 cases rose, many New England hospitals transferred their pediatric patients here.
“It was a win for everyone,” says Donald Bae, MD, clinical chief of orthopedic surgery. “The adult hospitals had more resources to treat their patients with COVID-19, and kids transferred here were only exposed to other kids.” Boston Children’s also provided ventilators to nearby hospitals overwhelmed by the outbreak. Many Boston Children’s respiratory therapists volunteered at these hospitals.
Lesson 3: Some elective procedures are not actually elective
Like other hospitals around the state, Boston Children’s announced the cancellation of elective procedures on March 16. There was not, however, a clear-cut way to decide which procedures were actually elective.
“Because of the specialized nature of this hospital, we couldn’t enforce a strict set of guidelines,” says Fishman. Instead, department chiefs and their teams determined — on a patient-by-patient basis — which procedures could be postponed without jeopardizing their patients’ outcomes.
The painstaking process paid off. Of the 24 ORs on Boston Children’s main campus, only six to eight were in use on any given day during the first outbreak. The hospital also scaled back the number of personnel in the OR. Research assistants stopped observing procedures in person and the hospital reduced its number of surgical trainees.
Whenever possible, patients’ pre-operative and post-operative appointments took place by virtual visit. “Telemedicine made it possible for us to see our patients without putting them at risk,” says Bae.
Lesson 4: Reopening may not mean business as usual
In mid-May, Boston Children’s started a slow, methodical process of reopening. By then, our backlog of procedures numbered in the thousands. Some operations that had been elective in March were becoming urgent. Starting with these patients, departments began rescheduling procedures, often in the evenings and on weekends. Throughout this time, we never eased up on universal masking, heightened use of PPE, health attestations, and other measures to protect our patients, families, and clinicians from infection.
And with the pandemic still ongoing, some resources remained in reserve. “We have kept one OR reserved for patients with COVID-19 who need emergency surgery,” says Fishman. “Those cases require special decontamination and extra time between operations.”
Lesson 5: COVID-19 safety measures remain critical
As many officials feared, cases of COVID-19 started to surge again in the fall. On December 7, Massachusetts Governor Charlie Baker ordered hospitals to curtail inpatient elective surgical operations. Once again, hospitals need to keep beds and equipment available for patients with COVID-19.
Boston Children’s safety measures during COVID-19
- universal masking for staff, clinicians, patients, and visitors
- eye protection for clinicians and staff interacting with patients
- mandatory health attestation before entering any facility
- plexiglass barriers in surgical waiting areas and throughout hospital
- telehealth consultations for pre- and post-op visits when clinically appropriate
- preoperative COVID-19 testing for all surgical patients
- plastic barriers in the OR during aerosol-generating procedures
- essential personnel only in the OR
This time around, Boston Children’s knows much more about the virus and how to prevent transmission. Guidelines and infrastructure remain in place to keep patients, families, and employees safe. The hospital’s vaccination program is also well underway, adding another layer of safety that was not available in the spring of 2020.
“We accomplished a great many things in a very short time,” says Fishman. “I think we’ve learned that sometimes the best way to get something done is to decide on the goals, decide which teams are best equipped to achieve those goals, and empower them to do the right thing.”
The response also demonstrates how a clear set of goals can unite a team. “We prioritized patient care, we took great care of kids, we never stopped providing emergency and urgent care, and we did it safely,” says Bae. “We will continue to do that throughout the pandemic.”
Learn more about Boston Children’s response to COVID-19 and more about the Department of Surgery and Orthopedic Center.
Related Posts :
-

Hip reconstruction in complex patients: Predicting complications
Neuromuscular hip dysplasia and progressive spastic hip displacement are among the most common orthopedic concerns in non-ambulatory children with cerebral ...
-

Spinal fusion surgery during COVID-19
If things had gone according to plan, Jared Cohen would have had spinal fusion surgery during his April vacation. His ...
-

Provider Spotlight: Meet Dr. Steve Fishman
How did you become interested in pediatric surgery? I became interested in pediatric surgery when I was first exposed ...
-

Lessons learned performing telehealth visits during COVID-19
In the midst of the COVID-19 pandemic, one positive development is that many health care providers are finding new ways ...





