Does cannabis affect surgical outcomes? We need more data.
After alcohol, marijuana is the most commonly used recreational substance among U.S. adults and adolescents. Up to 22 million Americans 12 or older use cannabis. In a 2022 survey by the National Institute on Drug Abuse, 0.7 percent of 8th graders, 2.1 percent of 10th graders, and 6.3 percent of 12th graders reported using marijuana 20 times or more in the past 30 days.
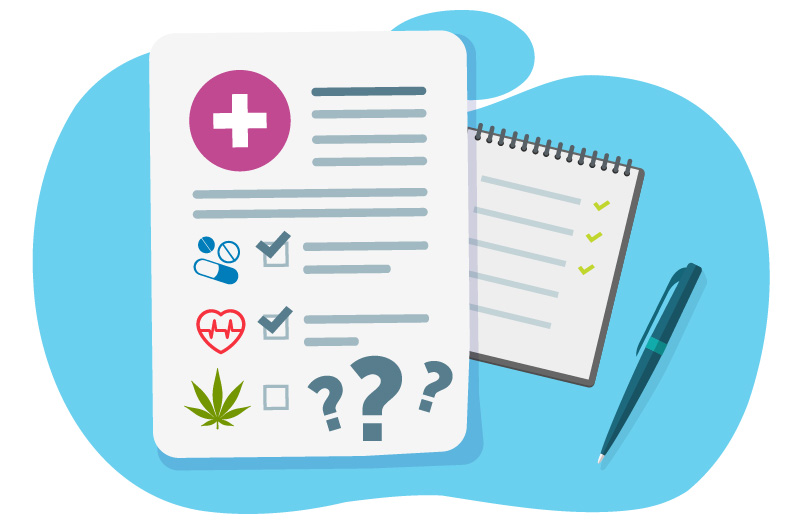
For pediatric surgeons, such statistics mean it’s likely some of their patients have cannabis in their systems. Yet questions about a patient’s marijuana use are not standard on pre-operative patient intake forms or any other preoperative documentation at children’s hospitals. The resulting lack of data hampers research into the ways cannabis may affect pediatric patients’ surgical outcomes — and orthopedic surgery is no exception.
Marijuana, bone healing, and data gaps
For example, some research suggests that cannabis use slows bone healing: In a 2021 study, orthopedic surgeon Grant Hogue, MD, of Boston Children’s Spine Division, and his colleagues analyzed results of urine toxicology screenings of adolescent trauma patients who underwent surgery for extremity (arm or leg) fractures at a hospital in Texas. In patients with positive cannabis screening results, the average time to bone union was 159 days, nearly twice as long as the average 80 days in patients with negative tests.
Most children’s hospitals don’t routinely perform urine toxicology screenings, however, and there’s much more we still don’t know about the effects of cannabis on surgical outcomes. “In theory, people who use marijuana daily or weekly may have more post-operative nausea and adverse pain responses,” says Hogue. “It may also slow fusion in spine patients, but we don’t have definitive evidence proving that.”
Measure it so you can manage it
That’s why Hogue and his colleague, Ata Kiapour, PhD, MMSc, director of Boston Children’s Musculoskeletal Informatics Group, are leading the charge to provide orthopedic surgeons with more insight into pediatric cannabis use. The first step: Assess the current state of data.
Using artificial intelligence (AI), they evaluated trends and disparities in cannabis documentation in pediatric orthopedic surgeries dating from 2000 to 2021. With almost 24 million clinical notes to assess, Kiapour and his team created a natural language processing (NLP) model to extract any instances of cannabis use documentation, including derivatives and misspellings, from unstructured clinical notes. This use of AI made it possible to study a large volume of unstructured data.
Their resulting work — published in npj digital medicine and one of the most comprehensive efforts to evaluate cannabis documentation in a large collection of clinical notes — found that less than 7 percent of patients were asked about and less than 2 percent self-reported cannabis use. By comparison, in Hogue’s previous study of adolescent trauma patients in Texas who underwent urine screening, more than 6 percent screened positive.
A call to action for health systems
These findings, Hogue and Kiapour say, are a call for health care providers to expand and standardize collection of patients’ substance use data.
Some surgeons ask their patients about substance use. But the brevity of most surgeon-patient interactions makes it challenging to establish the kind of trust necessary for an underage patient to divulge marijuana use, particularly with their parent or guardian in the room. For his part, Hogue talks with each patient ahead of their procedure about things they can do to support healing, including avoiding substances like cannabis.
But to address the data gap effectively, changes need to take place at a systems-wide level. One place to start: patient intake forms. “Intake forms at pediatric hospitals typically ask about smoking and drinking,” says Kiapour. “They don’t take into account cannabis, vaping, or psychedelics.”
Gathering such information can improve care: If a surgeon knows a patient uses marijuana, they can refer the patient to social work, counseling, or a cessation program before scheduling a procedure. It will also enable more research.
Hogue and Kiapour are forging ahead in that area. They’ve initiated retrospective studies of postoperative differences in orthopedic patients who attest to using marijuana compared to those who don’t. In a trio of studies, they’ll be looking at complications and pain scores following ACL reconstruction, periacetabular osteotomy, and spinal fusion (for adolescent idiopathic scoliosis). From there, prospective studies will follow.
Learn more about the Spine Division, Musculoskeletal Informatics Group, or refer a patient.
Related Posts :
-

AI could change the way we look at hip preservation
Orthopedic surgeons and biomedical engineers are trained to approach adolescent and young adult hip pain from two different perspectives. Surgeons ...
-

The surprisingly specific genetics of joint disease
A new study provides unexpected insights into the biology of two common, heritable orthopedic conditions: developmental dysplasia of the hip (...
-

Uncertainty surrounds ACL treatment decisions in young athletes. It shouldn’t.
It’s an injury once seen mainly in adults, yet it’s become increasingly common in younger patients. From 2000 to 2020, ...
-

Robotics, spinal fusion, and the quest for 100 percent accuracy
In any spinal fusion surgery, accurate screw placement is a top priority, and for good reason. Incorrectly positioned screws are ...